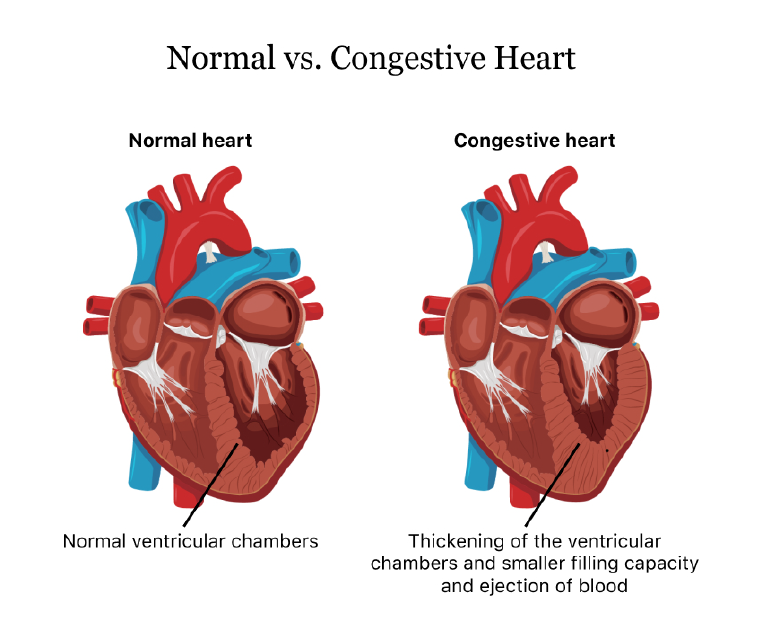
Congestive heart failure (CHF) is a condition in which the heart is unable to pump blood effectively to meet the body’s needs. This results in a build-up of fluid in the lungs, liver, and other tissues, leading to symptoms such as shortness of breath, fatigue, and swelling in the legs and ankles.
CHF can be caused by a variety of factors, including coronary artery disease, high blood pressure, and valve disorders. It can also occur as a result of certain medical conditions, such as diabetes, obesity, and thyroid disorders. Lifestyle factors such as smoking, excessive alcohol consumption, and lack of exercise can also increase the risk of CHF.
Symptoms
Symptoms of CHF can vary depending on the severity of the condition and the underlying cause. Some of the most common symptoms include:
- Shortness of breath: This is often the first symptom of CHF and can occur even during normal activities such as walking or climbing stairs. The shortness of breath can be accompanied by coughing or wheezing.
- Fatigue: People with CHF often experience extreme tiredness, even after minimal physical activity.
- Swelling: Fluid build-up in the legs, ankles, and feet can cause swelling, also known as edema. This can also occur in the abdomen and other areas of the body.
- Rapid heartbeat: CHF can cause the heart to beat faster than normal in an attempt to compensate for the decreased pumping ability.
- Decreased appetite: CHF can cause a loss of appetite and nausea, which can lead to weight loss.
If left untreated, CHF can lead to serious complications such as kidney failure, liver damage, and even death. However, with proper treatment and management, many people with CHF can live healthy and active lives.
Diagnosis & Treatment
Diagnosis of CHF typically involves a physical exam, medical history, and diagnostic tests such as chest x-rays, electrocardiograms (ECGs), and echocardiograms. These tests can help identify the underlying cause of the condition and determine the extent of the damage to the heart.
Treatment for CHF typically involves a combination of lifestyle changes, medications, and in some cases, surgical procedures. Some of the most common treatments for CHF include:
- Medications: Medications such as diuretics, ACE inhibitors, and beta-blockers can help reduce fluid build-up, lower blood pressure, and improve heart function.
- Lifestyle changes: Lifestyle changes such as quitting smoking, reducing alcohol consumption, and maintaining a healthy weight can help improve heart function and reduce the risk of complications.
- Cardiac rehabilitation: This is a supervised exercise program designed to help people with CHF improve their fitness levels and overall health.
- Implantable devices: Devices such as pacemakers and implantable cardioverter-defibrillators (ICDs) can help regulate the heartbeat and prevent dangerous heart rhythms.
- Surgery: In some cases, surgery may be necessary to repair or replace damaged heart valves or to bypass blocked arteries.
Conclusion
While CHF is a serious condition, there are many things that people with the condition can do to improve their overall health and quality of life. This includes consuming a healthy diet, regular exercise, avoiding smoking and excessive alcohol consumption. It is also important for people with CHF to consult their doctor regularly for monitoring of symptoms and medication adjustments as needed. By adopting these measures, people with CHF can manage their symptoms and reduce their risk of complications.