The left ventricle is a crucial component of the human heart, playing a vital role in pumping oxygenated blood to the rest of the body. It is one of the four chambers of the heart and is responsible for the majority of the heart’s pumping action.
Anatomy
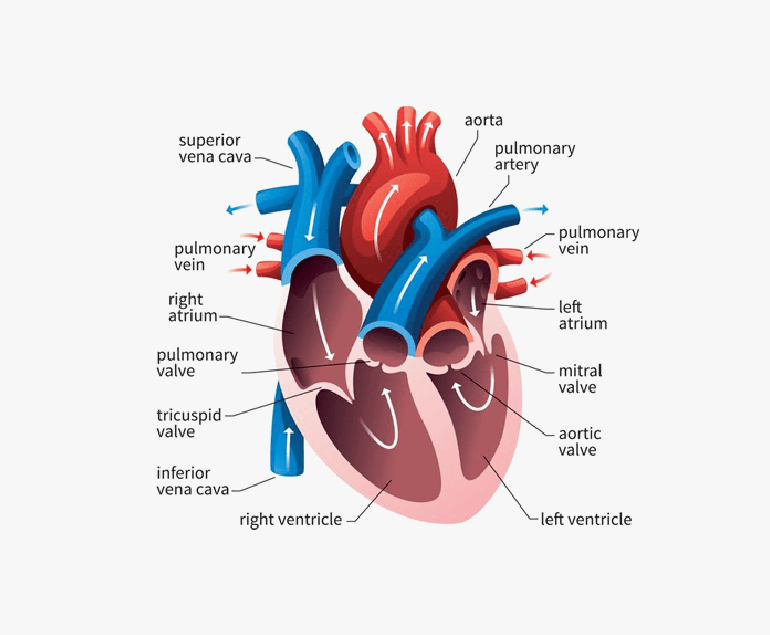
The left ventricle is located at the bottom left side of the heart and is the largest and thickest chamber. It is responsible for receiving oxygen-rich blood from the left atrium and pumping it out to the body through the aorta, the largest artery in the body.
The walls of the left ventricle are highly muscular and contract forcefully during each heartbeat to propel blood into the circulation.
Function
The primary function of the left ventricle is to generate enough force to pump blood to the entire body. It achieves this by contracting and relaxing in a coordinated manner with the other chambers of the heart. During systole, the contraction phase, the left ventricle contracts forcefully, pushing blood into the aorta.
This blood is then distributed to various organs and tissues, delivering oxygen and nutrients essential for their functioning. In diastole, the relaxation phase, the left ventricle refills with blood from the left atrium, preparing for the next contraction.
Significance of the Left Ventricle
The left ventricle is often referred to as the “workhorse” of the heart due to its critical role in maintaining the circulation of oxygenated blood throughout the body. Its muscular walls are much thicker than those of the other chambers, enabling it to generate the necessary force for pumping blood against the high resistance of the systemic circulation. The left ventricle’s ability to contract forcefully is crucial for maintaining adequate blood flow and oxygen supply to the body’s organs and tissues.
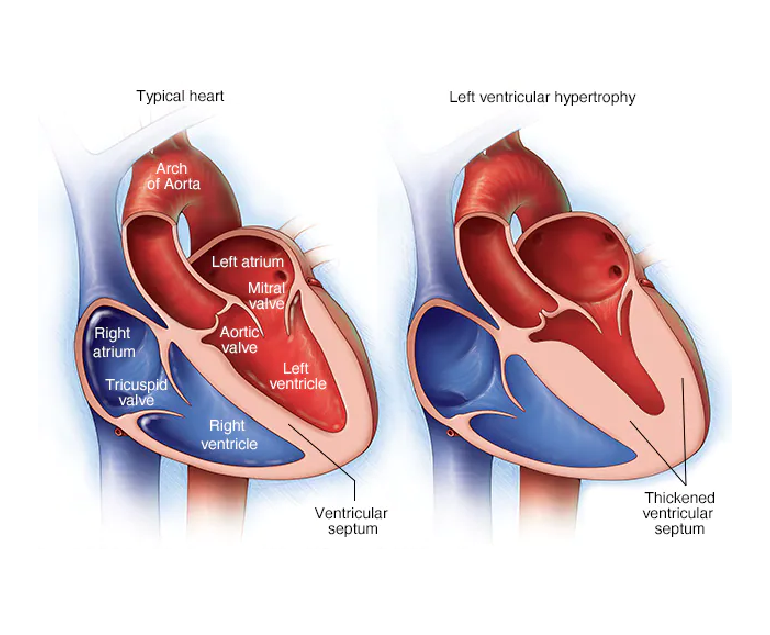
In addition, the left ventricle is intricately connected to various aspects of cardiovascular health. It is commonly assessed through medical imaging techniques such as echocardiography and cardiac MRI to evaluate its size, shape, and function. Changes in the structure or function of the left ventricle can indicate underlying heart conditions, such as left ventricular hypertrophy, heart failure, or coronary artery disease. By monitoring the left ventricle’s health, medical professionals can diagnose and manage these conditions more effectively.
Maintaining a Healthy Left Ventricle
Managing risk factors such as high blood pressure, high cholesterol levels, obesity, and diabetes is essential in preventing left ventricular dysfunction. These conditions can put undue strain on the heart and lead to the development of cardiovascular diseases. Lifestyle modifications, medication, and close monitoring by healthcare professionals can help control these risk factors and preserve the optimal function of the left ventricle.
Conclusion
The left ventricle is a crucial component of the heart, responsible for pumping oxygenated blood to the body’s organs and tissues. Its powerful contractions and thick muscular walls enable it to generate the force necessary for systemic circulation.
Monitoring and maintaining the health of the left ventricle are vital in preventing and managing heart conditions. By adopting a healthy lifestyle, managing risk factors, and seeking regular medical care, individuals can support the proper functioning of the left ventricle and promote overall cardiovascular well-being.