Patent ductus arteriosus is a very common heart condition found in new born babies. It occurs because the ductus arteriosus blood vessel doesn’t close properly after birth.
Babies born prematurely are more likely to be affected by PDA. The risk of PDA increases the earlier the baby is born. PDA affects 10% of babies born between 30 and 37 weeks of pregnancy, 80% of babies born between 25 and 28 weeks of pregnancy and 90% of babies born earlier than 24 weeks of pregnancy.
PDA is also more commonly seen in girls than in boys.
Cause of PDA
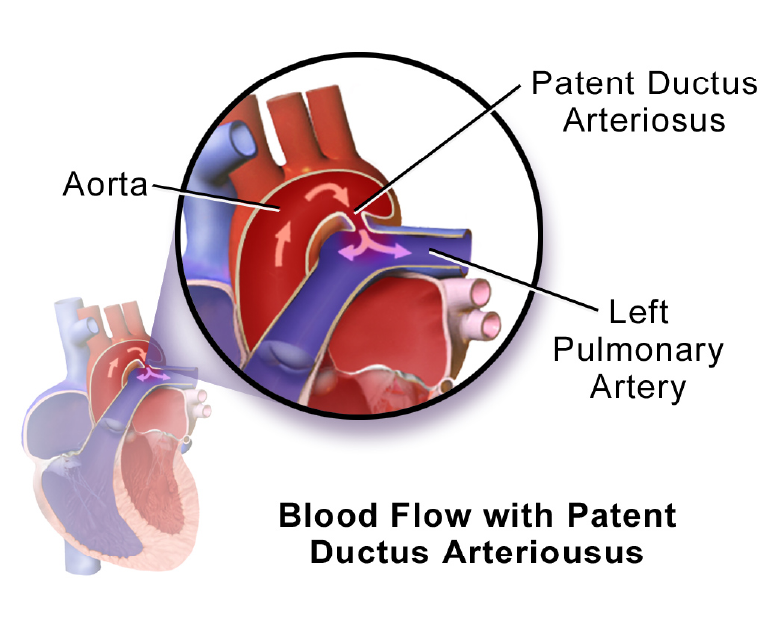
Every baby has a ductus arteriosus, which is a foetal artery connecting the aorta and the pulmonary artery. This opening usually narrows and closes within a few days after birth. If it continues to remain open it is known as patent ductus arteriosus (PDA).
While a small PDA may not generally cause any problems, a large PDA can lead to the flow of poorly oxygenated blood in the wrong direction. This can cause heart failure and other complications such as pulmonary hypertension and blood vessel damage.
Causes of PDA include genetic disorders or a family history of the condition. Babies with neonatal respiratory distress syndrome which is a breathing problem or those born to mothers who had rubella during pregnancy are also at risk of developing PDA.
Symptoms
PDA symptoms vary according to the size of the defect. Small PDAs may not have symptoms apart from a heart murmur and may go undetected until adulthood.
Large PDAs may cause symptoms such as:
- Persistent rapid breathing.
- Breathlessness
- Sweating often
- Fatigue
- or tiredness
- Feeding and eating problems
- Poor weight gain
- Rapid heart rate
It is important to consult a doctor immediately if any of these symptoms are noticed in the baby.
Diagnosis and Treatment
PDA in premature babies and in neonates may be the cause of respiratory compromise. Many a time’s medicine is effective. In cases where medicine has failed or cannot be given due to many reasons, surgery is required.
The paediatric cardiologist may recommend various tests such as Chest X-ray, Electrocardiogram (ECG), Echocardiogram, etc to diagnose the PDA.
A small PDA may close on its own as the child grows and may not require treatment. Doctors will prescribe the medication as required.
Large PDAs may require treatment that includes cardiac catheterization or surgery. Catheterization is a minimally invasive procedure where the doctors use a flexible tube or catheter and insert a coil through it into the heart to close the PDA. In PDA surgery an incision is made to the side of the chest and the PDA is closed with stiches or a metal clip.
Life after PDA treatment
After receiving treatment for PDA, children can lead normal, healthy lives. Activity levels, appetite, and growth will return to normal within a short duration. Periodic check-ups with the paediatric cardiologist will ensure that there are no heart or lung problems.