Aging and Heart Disease are interconnected in several ways. As individuals age, their chances of developing heart disease increase. Aging is associated with various physiological changes that can affect the cardiovascular system. Here are some key points to consider regarding heart disease and aging:
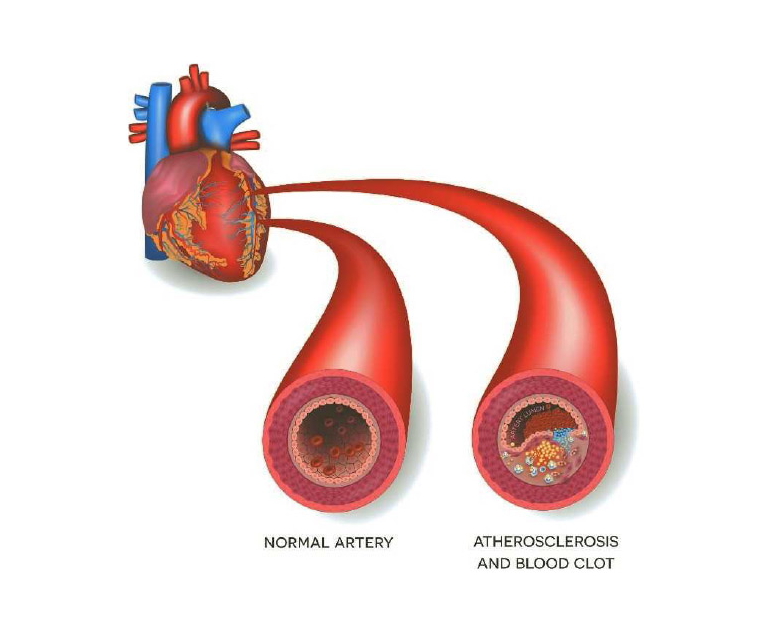
Atherosclerosis: Aging often leads to the accumulation of fatty deposits (plaque) in the arteries, a condition known as atherosclerosis. This buildup can narrow and stiffen the arteries, reducing blood flow to the heart and increasing the risk of heart disease.
Blood Vessel Changes: With aging, blood vessels may become less flexible and more prone to stiffness. This can contribute to high blood pressure (hypertension), which is a significant risk factor for heart disease.
Heart Muscle Changes: The heart undergoes changes with age, including a gradual thickening of the heart walls and a decrease in the elasticity of the heart chambers. These changes may affect the heart’s ability to pump blood efficiently.
Collagen Accumulation: Collagen, a protein that provides structure to various tissues, accumulates in the heart with age. This can contribute to the stiffening of the heart muscle and impaired cardiac function.
Inflammation: Chronic low-grade inflammation is associated with aging and is also a factor in the development of heart disease. Inflammatory processes can contribute to the progression of atherosclerosis and other cardiovascular issues.
Metabolic Changes: Changes in metabolism, such as alterations in lipid (fat) profiles and glucose metabolism, are common with aging. These changes can influence the development of conditions such as diabetes and metabolic syndrome, which are risk factors for heart disease.
Genetic and Environmental Factors: Both genetic and environmental factors play a role in the development of heart disease. Aging individuals may have a combination of genetic predispositions and a lifetime of exposure to various risk factors, such as a poor diet, a sedentary lifestyle, and smoking.
Hormonal Changes: Hormonal changes, especially in postmenopausal women, can contribute to an increased risk of heart disease. Estrogen, which has cardioprotective effects, decreases with age and menopause.
Lifestyle Factors: Healthy lifestyle choices, such as a balanced diet, regular physical activity, maintaining a healthy weight, and avoiding smoking, can help mitigate the risk of heart disease even as individuals age.
Medical Monitoring and Management: Regular medical check-ups and monitoring of blood pressure, cholesterol levels, and other cardiovascular risk factors are crucial, especially as people age. Timely intervention and management of risk factors can help prevent or delay the onset of heart disease.
It’s important to note that while aging is a non-modifiable risk factor, adopting a healthy lifestyle and managing other risk factors can significantly influence heart health and reduce the impact of age-related changes on the cardiovascular system. Regular consultation with healthcare professionals is essential for monitoring and managing cardiovascular health, especially in older individuals.