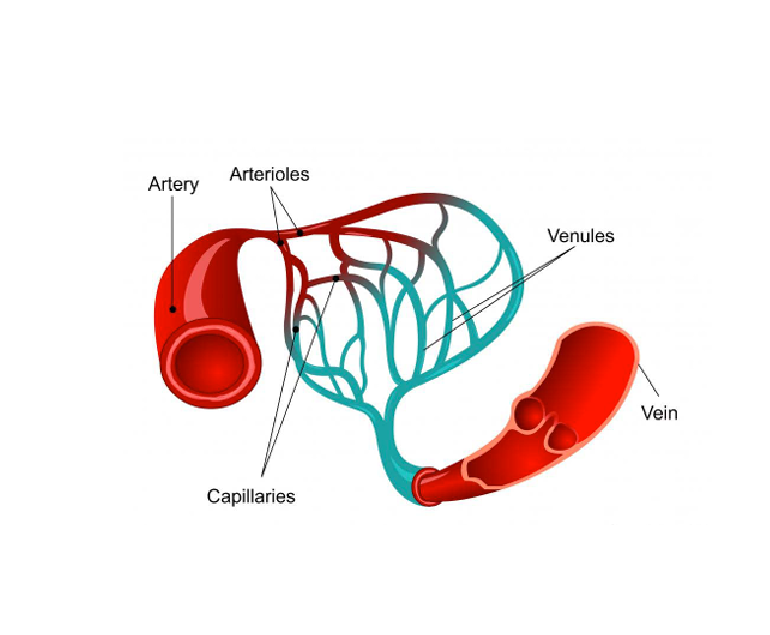
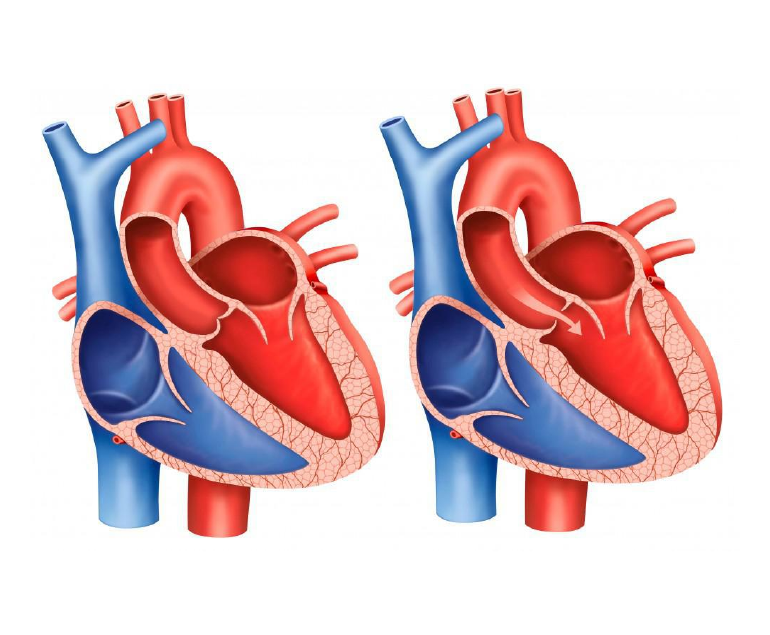
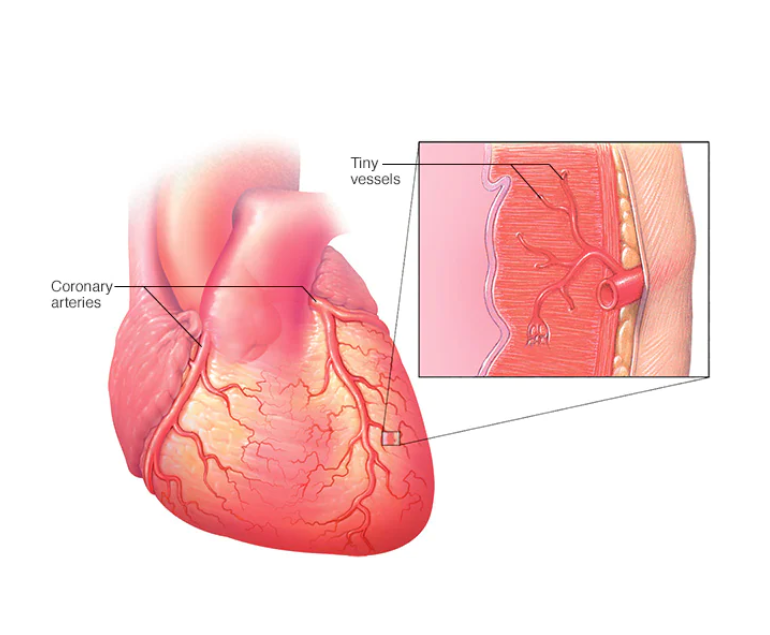
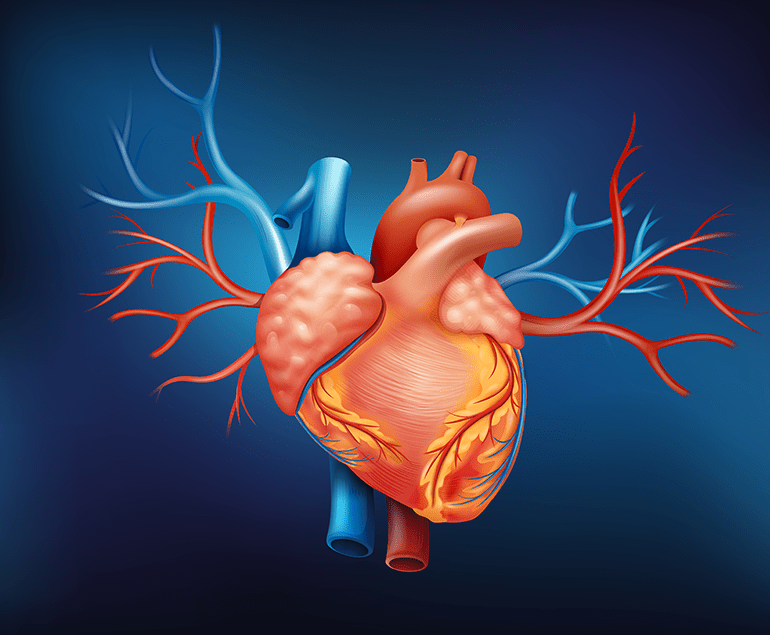
Vasculitis is a medical condition that affects the blood vessels in the body, leading to inflammation and damage to these vital structures. The blood vessels affected by vasculitis can range from small capillaries to larger arteries, depending on the type of vasculitis. This damage to the blood vessels can cause a range of symptoms and health problems, including impaired blood flow, organ damage, and increased risk of infections and bleeding.
Types of Vasculitis
There are several different types of vasculitis, each with its own unique causes, symptoms, and treatment options. Some of the most common types of vasculitis include giant cell arteritis, Takayasu’s arteritis, and Wegener’s granulomatosis. These diseases can affect people of all ages, and can be caused by a variety of factors, including infections, autoimmune disorders, and exposure to certain medications or chemicals.
Symptoms
The symptoms of vasculitis can vary widely, depending on the type and severity of the disease, as well as the location of the affected blood vessels. Some common symptoms of vasculitis include fever, fatigue, weight loss, joint pain, skin rashes, and sores that do not heal. In severe cases, vasculitis can also cause organ damage, such as kidney failure, heart attack, or stroke.
Diagnosis and Treatment
Diagnosing vasculitis can be challenging, as the symptoms can be similar to other diseases and conditions. The process usually involves a thorough medical history, physical examination, blood tests, and imaging studies, such as MRI or CT scans. In some cases, a biopsy may be necessary to confirm the diagnosis.
Treatment for vasculitis depends on the type and severity of the disease, as well as the age and overall health of the patient. In many cases, treatment involves a combination of medications, such as corticosteroids and immunosuppressants, to reduce inflammation and prevent further damage to the blood vessels. These medications can be taken orally or intravenously, and may need to be taken for an extended period of time.
In severe cases of vasculitis, treatment may also involve other interventions, such as stents, surgery or radiation therapy. For example, if the vasculitis is causing a blockage in a major blood vessel, such as the aorta, surgery may be necessary to remove the blockage and restore normal blood flow.
Living with vasculitis
Living with vasculitis can be challenging, but with proper treatment and care, many people are able to manage their symptoms and lead healthy lives. It is important to consult a specialist and monitor your symptoms and medical condition regularly. This may include regular blood tests, imaging studies, and physical exams, as well as lifestyle changes, such as maintaining a healthy diet and getting regular exercise.
Conclusion
Vasculitis is a group of rare diseases characterized by inflammation and damage to the blood vessels in the body. The symptoms and treatment options can vary widely depending on the type and severity of the disease, but with proper care and management, many people are able to live active, healthy lives.