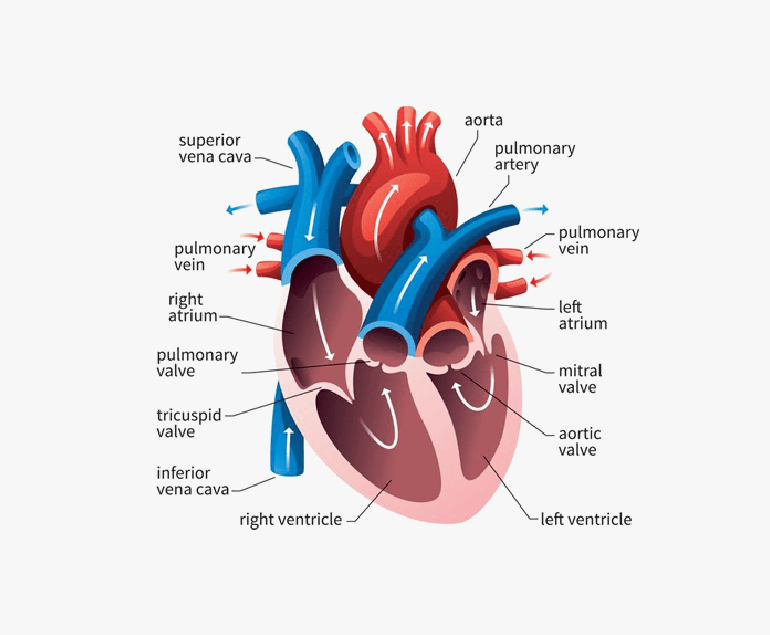
The human heart is an extraordinary organ, tirelessly pumping blood throughout our bodies. At the core of this remarkable organ are four crucial valves that ensure the unidirectional flow of blood, maintaining the delicate balance of oxygen and nutrients. However, when these valves become compromised due to diseases or congenital abnormalities, it can lead to life-threatening conditions. Dr. Ramji Mehrotra, who is widely regarded as the Best Heart Specialist Doctor in India, is of the opinion that prosthetic heart valves have emerged as a groundbreaking solution, offering hope to patients facing valve-related heart disorders.
Prosthetic heart valves, also known as artificial heart valves, are medical devices designed to replace the natural heart valves when they are no longer functioning properly. These devices are indispensable in the field of cardiology, serving as a lifeline for countless individuals affected by valvular diseases. There are two primary types of prosthetic heart valves: mechanical and biological.
Mechanical heart valves are typically constructed from durable materials like titanium, carbon, or stainless steel. They are known for their longevity and robustness, often lasting for decades. However, one of the drawbacks of mechanical valves is the increased risk of blood clot formation. Patients with mechanical valves need to take anticoagulant medications for the rest of their lives to prevent clotting, which can lead to serious complications such as strokes.
On the other hand, biological heart valves are derived from either animal tissues (xenografts) or human tissues (homografts or allografts). These valves closely mirror the natural valve structure and are less likely to cause blood clotting. However, they have a limited lifespan and may need to be replaced after 10-15 years, depending on factors like patient age and activity level.
The choice between mechanical and biological prosthetic heart valves depends on various factors, including the patient’s age, lifestyle, and overall health. Younger patients may opt for mechanical valves due to their longevity, while older patients may prefer biological valves to avoid the long-term use of anticoagulants. The decision is often made in consultation with a cardiac surgeon and is tailored to the individual patient’s needs.
Prosthetic heart valve surgery is a complex and highly specialized procedure. It involves the removal of the damaged natural valve and the implantation of the artificial valve. Open-heart surgery has traditionally been the standard approach for valve replacement, but minimally invasive techniques are gaining popularity, offering shorter recovery times and reduced postoperative pain.
Dr.Mehrotra says that the development of prosthetic heart valves has significantly improved the quality of life for patients with valvular heart diseases. It has not only extended the lifespan of individuals facing life-threatening conditions but has also enhanced their overall well-being. These artificial valves restore normal blood flow, relieve symptoms like shortness of breath and fatigue, and allow patients to engage in physical activities they might have previously been unable to enjoy.
In conclusion, prosthetic heart valves have revolutionized the field of cardiology, providing a lifeline to individuals suffering from valvular heart diseases. Whether mechanical or biological, these artificial valves have saved countless lives and improved the quality of life for many more.