Truncus arteriosus is a rare congenital heart defect that occurs in approximately 1 in 10,000 live births. It is a serious condition that requires prompt medical attention and intervention to prevent potentially life-threatening complications.
What is Truncus arteriosus?
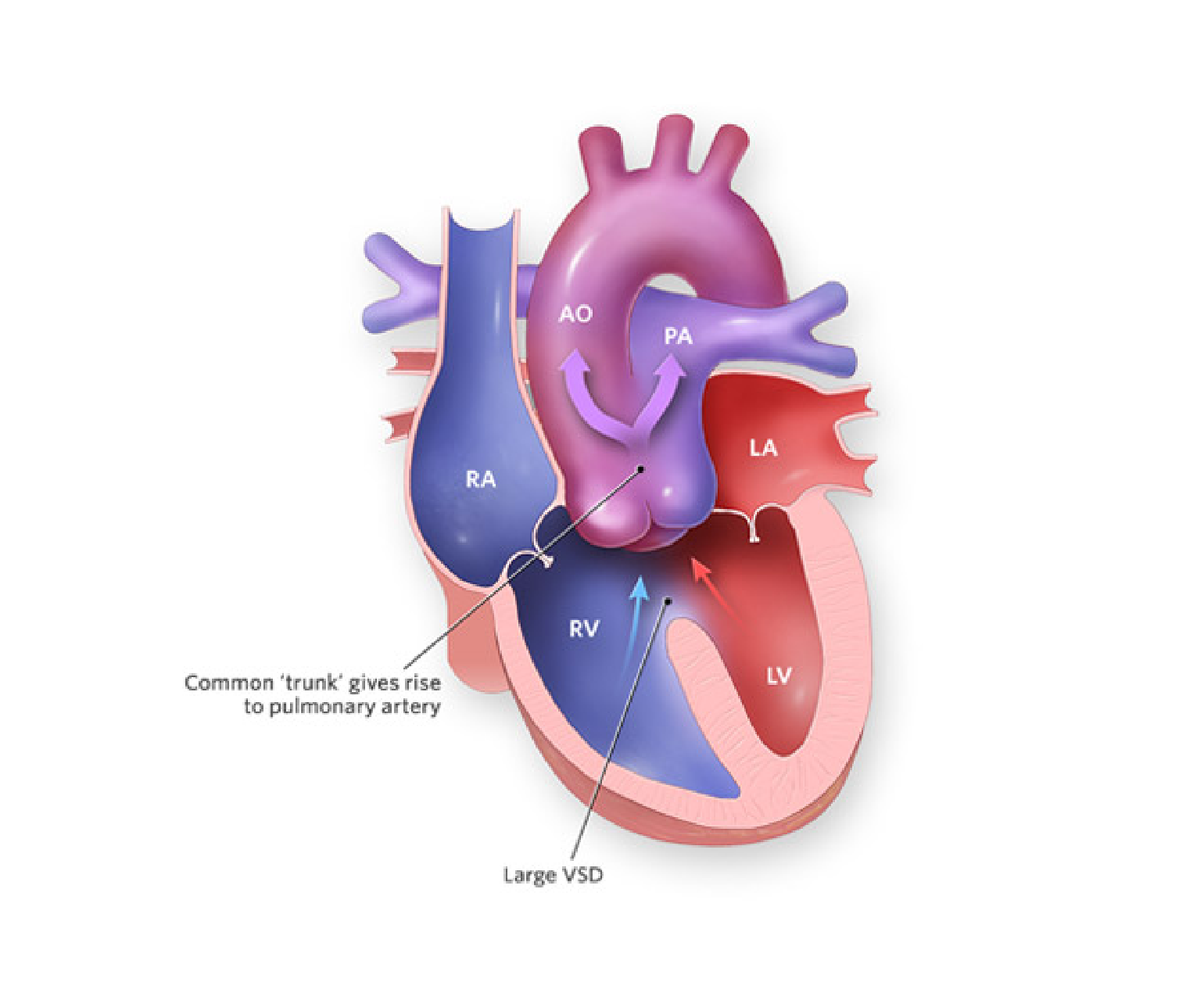
In a normal heart, the blood is pumped from the right side of the heart to the lungs, where it is oxygenated, and then returned to the left side of the heart, where it is pumped out to the rest of the body. This process is facilitated by two separate arteries, the pulmonary artery, which carries blood to the lungs, and the aorta, which carries blood to the rest of the body.
However, in the case of truncus arteriosus, the pulmonary artery and the aorta fail to separate during foetal development, resulting in a single large vessel that arises from both the right and left ventricles. This vessel is known as the truncus arteriosus. Additionally, there is usually a hole in the wall that separates the ventricles, called a ventricular septal defect (VSD).
As a result of this defect, oxygen-rich and oxygen-poor blood mix together in the truncus arteriosus before being pumped out to the body. This results in a lack of oxygen to the body’s tissues, leading to symptoms such as fatigue, shortness of breath, and poor growth.
Truncus arteriosus can also lead to more serious complications such as heart failure, pulmonary hypertension, and developmental delays. The severity of the condition depends on the size of the VSD and the degree of mixing of blood within the truncus arteriosus.
Diagnosis & Treatment
Truncus arteriosus is typically diagnosed soon after birth or during infancy, with symptoms such as a bluish tint to the skin (cyanosis), rapid breathing, and poor feeding. Diagnostic tests such as echocardiography, cardiac catheterization, and magnetic resonance imaging (MRI) may be performed to confirm the diagnosis and evaluate the severity of the defect.
Treatment for truncus arteriosus usually involves surgery to repair the defect. This surgery typically involves dividing the truncus arteriosus into two separate vessels, the pulmonary artery and the aorta, and patching the VSD. The timing of the surgery depends on the severity of the defect, but it is typically performed within the first few months of life.
Following surgery, regular follow-up appointments with a pediatric cardiologist are necessary to monitor the child’s progress and ensure that the repair is successful. Some children may require additional procedures or treatments, such as medication for pulmonary hypertension or developmental therapy for delays.
The prognosis for children with truncus arteriosus depends on the severity of the defect and the presence of any associated conditions. However, with prompt diagnosis, early intervention, and appropriate medical care, many children with truncus arteriosus go on to lead healthy, active lives.
Conclusion
Truncus arteriosus is a rare but serious congenital heart defect that requires prompt medical attention and intervention. Parents and caregivers should be aware of the symptoms and seek medical attention if they suspect their child may have this condition. With appropriate treatment and follow-up care, many children with truncus arteriosus can lead healthy, fulfilling lives.