The preoperative and postoperative care for Coronary Artery Bypass Grafting (CABG) is crucial for the overall success of the procedure and the patient’s recovery. Here’s an overview of the care provided before and after CABG:
Preoperative Care:
- Medical Evaluation:
- A thorough medical history and physical examination are conducted to assess the patient’s overall health and identify potential risks.
- Diagnostic tests, such as electrocardiogram (ECG), echocardiogram, and blood tests, help evaluate the extent and severity of coronary artery disease.
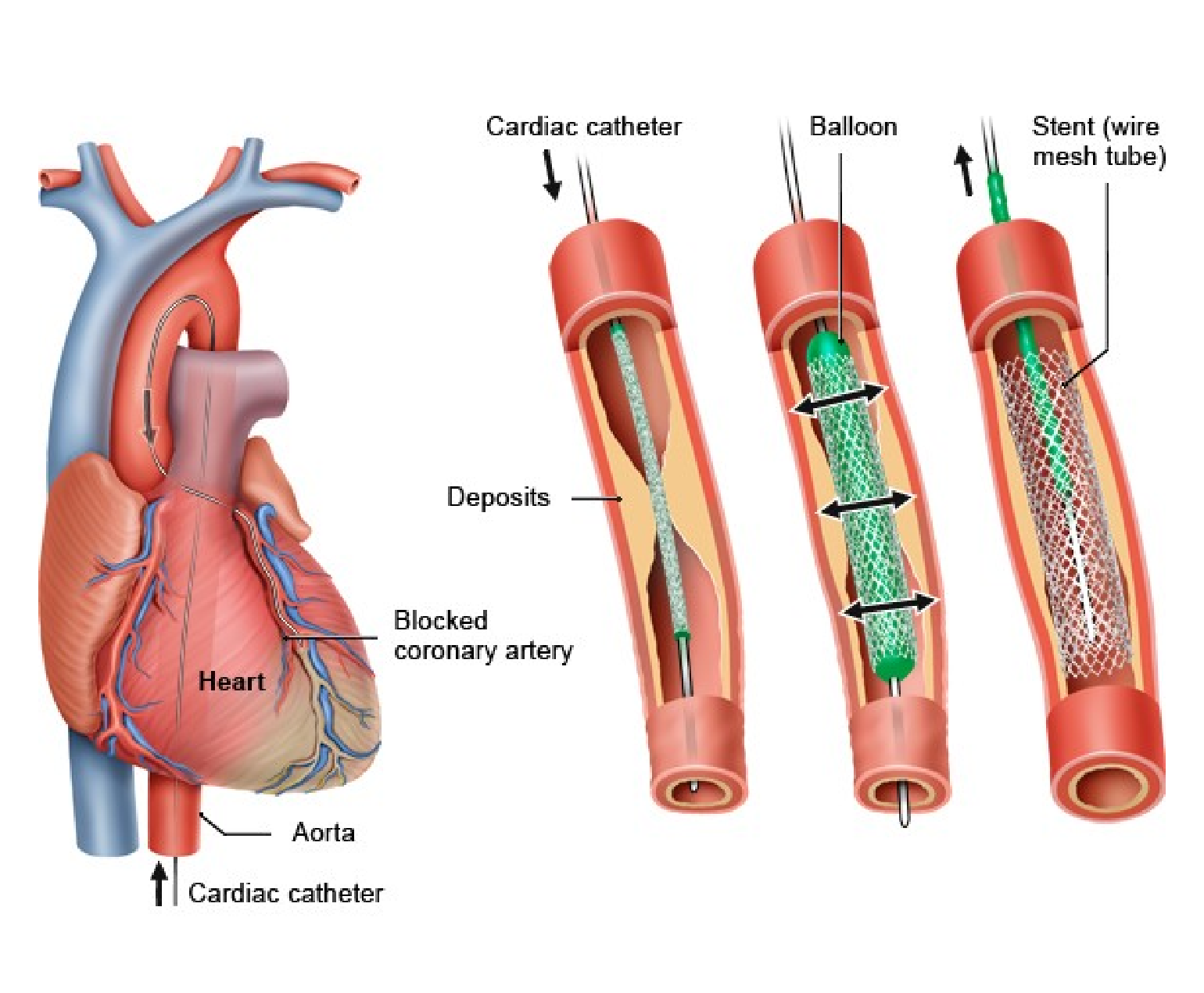
- Cardiac Catheterization and Angiography:
- Coronary angiography is often performed to visualize the coronary arteries and determine the location and severity of blockages.
- Coronary angiography is often performed to visualize the coronary arteries and determine the location and severity of blockages.
- Medication Management:
- Medications, such as antiplatelets and anticoagulants, may be prescribed to manage blood clotting and reduce the risk of complications.
- Medications, such as antiplatelets and anticoagulants, may be prescribed to manage blood clotting and reduce the risk of complications.
- Smoking Cessation:
- Patients are strongly encouraged to quit smoking before surgery to improve their overall cardiovascular health.
- Patients are strongly encouraged to quit smoking before surgery to improve their overall cardiovascular health.
- Dietary Guidelines:
- Dietary modifications may be recommended to manage cholesterol levels and optimize the patient’s nutritional status.
- Dietary modifications may be recommended to manage cholesterol levels and optimize the patient’s nutritional status.
- Preoperative Education:
- Patients receive information about the surgery, potential risks, and postoperative care.
- Rehabilitation plans and lifestyle changes are discussed.
Postoperative Care:
- Immediate Postoperative Period (ICU):
- Patients are closely monitored in the intensive care unit (ICU) initially.
- Vital signs, fluid balance, and cardiac function are closely observed.
- Pain Management:
- Adequate pain control is essential for patient comfort and to facilitate early mobility.
- Pain medications are administered as needed.
- Monitoring and Assessment:
- The continuous monitoring of heart rate, blood pressure, oxygen saturation, and other vital signs is necessary.
- Regular assessments of wound sites, neurological status, and respiratory function.
- Respiratory Care:
- Breathing exercises and incentive spirometry are encouraged to prevent complications like atelectasis and pneumonia.
- Early ambulation helps improve lung function.
- Medication Management:
- Medications, including antiplatelets, anticoagulants, and medications to control blood pressure and cholesterol, are prescribed as needed.
- Medications, including antiplatelets, anticoagulants, and medications to control blood pressure and cholesterol, are prescribed as needed.
- Nutritional Support:
- Nutritional needs are assessed, and a plan is developed to ensure the patient receives adequate nourishment for recovery.
- Nutritional needs are assessed, and a plan is developed to ensure the patient receives adequate nourishment for recovery.
- Rehabilitation and Physical Therapy:
- Gradual mobilization and physical therapy are initiated to improve strength and endurance.
- Cardiac rehabilitation programs may be recommended for long-term cardiovascular health.
- Follow-up and Lifestyle Changes:
- To monitor progress, it is necessary to have regular follow-up appointments with healthcare providers.
- Implementation of lifestyle changes, including a heart-healthy diet, regular exercise, and smoking cessation.
- Emotional Support:
- Psychological support is provided to help patients cope with the emotional aspects of surgery and recovery.
Both preoperative and postoperative care are collaborative efforts involving the surgical team, nurses, rehabilitation specialists, and the patient. The goal is to optimize the patient’s overall health, minimize complications, and support a successful recovery. Individual care plans may vary, and patients should follow the specific recommendations provided by their healthcare team.
Both preoperative and postoperative care are collaborative efforts involving the surgical team, nurses, rehabilitation specialists, and the patient. The goal is to optimize the patient’s overall health, minimize complications, and support a successful recovery. Individual care plans may vary, and patients should follow the specific recommendations provided by their healthcare team.