Heart disease is one of the leading causes of mortality and requires advanced medical interventions. Pericardiocentesis is a critical procedure in addressing complications related to pericardial effusion – a condition characterized by the accumulation of fluid in the pericardium, the protective sac around the heart. This procedure plays a vital role in both diagnosing and treating underlying heart conditions, alleviating symptoms, and preventing potentially life-threatening complications.
Causes
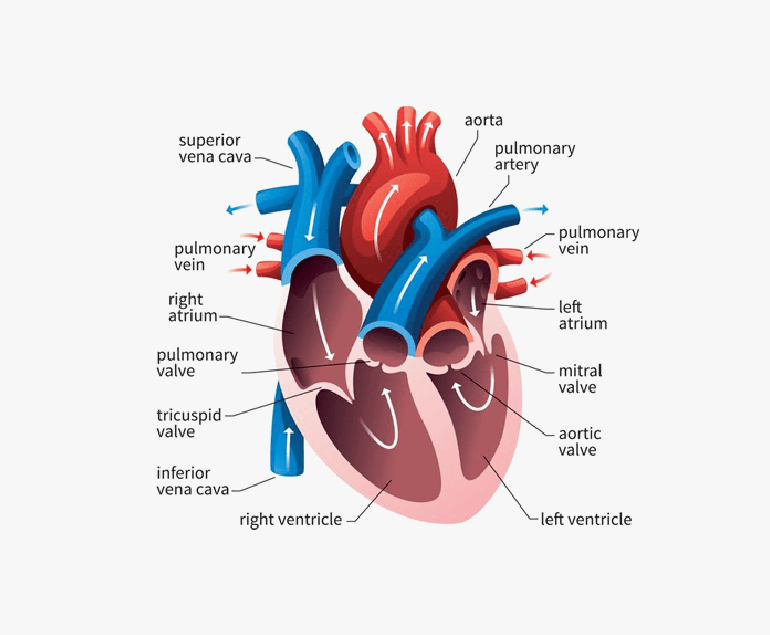
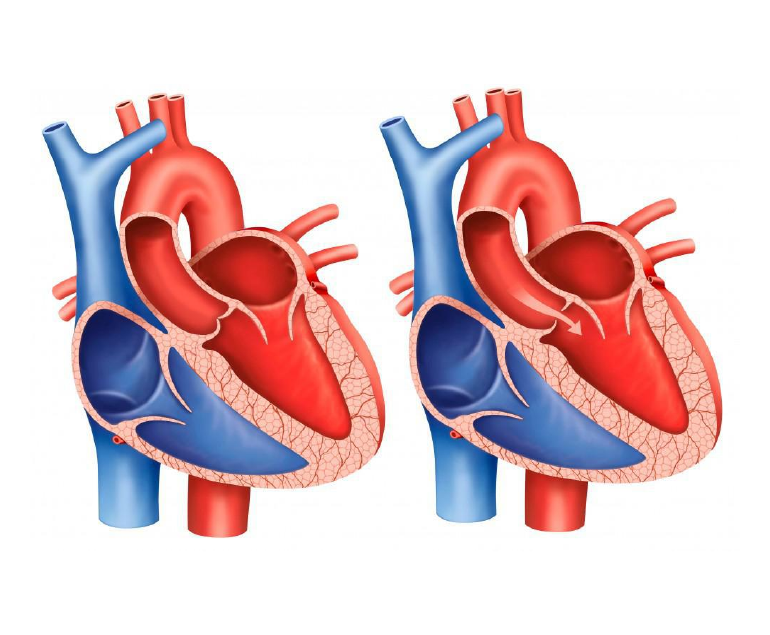
Pericardial effusion can result from various factors such as infections, inflammation, malignancies, trauma, or as a consequence of cardiac surgery. The accumulation of excess fluid within the pericardial space can exert pressure on the heart, impairing its ability to pump blood effectively. This can lead to symptoms like chest pain, shortness of breath, and even cardiac tamponade – a condition where the pressure from the fluid buildup compresses the heart chambers, compromising its function and circulation.
Procedure
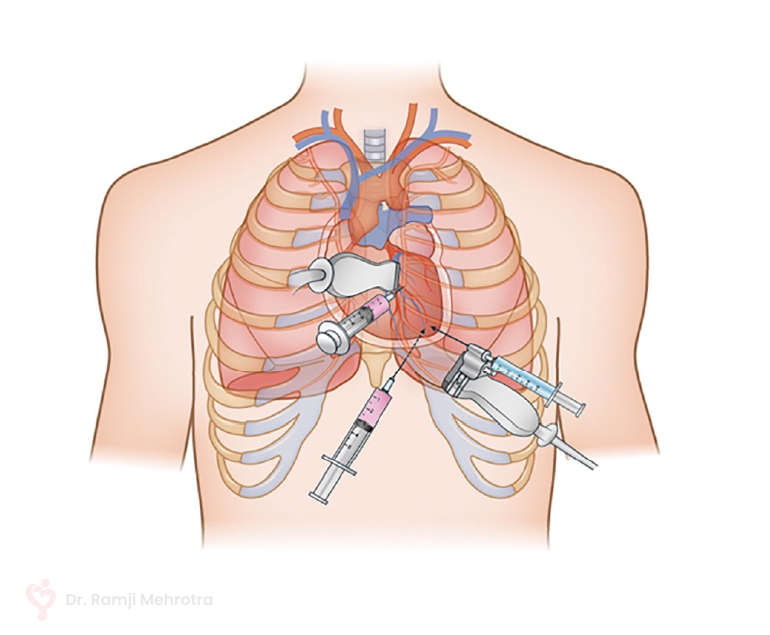
Pericardiocentesis involves the insertion of a needle or catheter into the pericardial space to drain the accumulated fluid. This procedure serves a dual purpose: providing symptomatic relief by relieving the pressure on the heart and facilitating diagnostic evaluation by analyzing the removed fluid for potential underlying causes.
The pericardiocentesis procedure is performed under imaging guidance, such as echocardiography or fluoroscopy, to ensure precision and minimize the risk of complications. The needle is carefully guided into the pericardial sac, and the fluid is aspirated. In some cases, a catheter may be left in place for continuous drainage if there is a significant fluid buildup or if the effusion is recurrent.
Benefits
Pericardiocentesis can provide rapid relief from the debilitating symptoms caused by pericardial effusion. By promptly reducing the pressure on the heart, patients often experience a marked improvement in their ability to breathe and reduced discomfort. Additionally, the removed fluid can be sent for analysis, which helps in diagnosing the underlying cause of the effusion. This diagnostic insight is crucial in guiding subsequent treatment decisions.
In some cases, pericardiocentesis may serve as a temporary measure while other interventions, such as medication, are initiated to address the underlying condition causing the effusion. However, in more severe cases where pericardial effusion poses an immediate threat to cardiac function, pericardiocentesis can be a life-saving intervention.
Conclusion
Pericardiocentesis plays a vital role in the management of heart disease, specifically in addressing the complications arising from pericardial effusion. This procedure offers both diagnostic and therapeutic benefits, helping in the swift mitigation of symptoms and potentially preventing life-threatening cardiac complications.