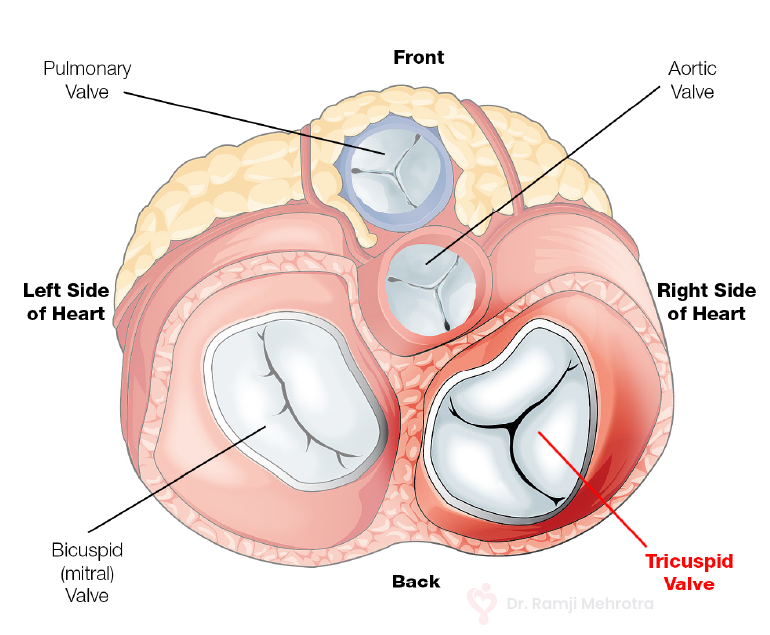
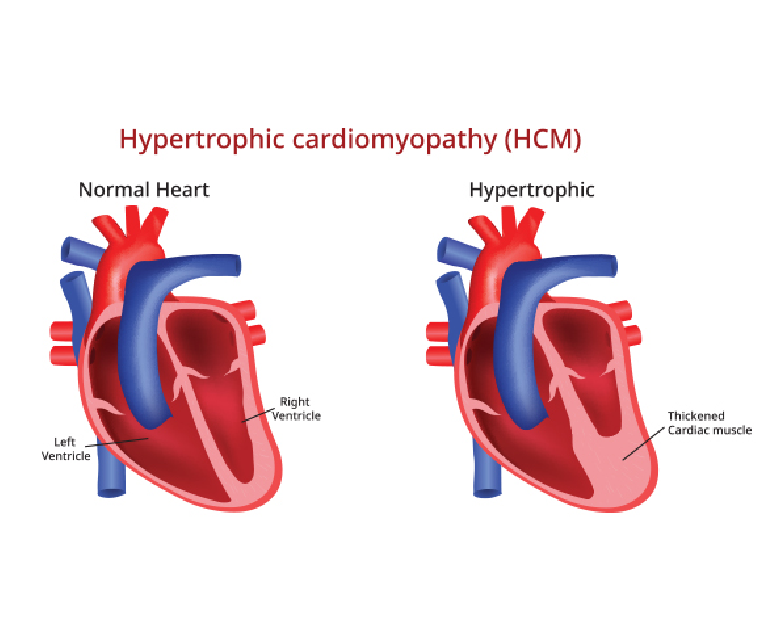
Pregnancy is a transformative and joyous experience in a woman’s life, but it also places significant physiological demands on the body. For women with pre-existing cardiovascular disease, pregnancy can present unique challenges and risks. Cardiovascular disease encompasses a range of conditions that affect the heart and blood vessels, including hypertension, congenital heart defects, valvular heart disease, and cardiomyopathy. Managing cardiovascular disease during pregnancy requires careful planning, monitoring, and collaboration between obstetricians and cardiologists to ensure the health of both the mother and the developing fetus.
Risk Factors and Preconception Care
Women with pre-existing cardiovascular disease who plan to become pregnant should receive specialized preconception care. This involves a thorough assessment of their cardiovascular health, including a review of their medical history, current medications, and cardiac function. Understanding the specific type and severity of cardiovascular disease is essential for risk assessment and management planning.
Risks for Mother
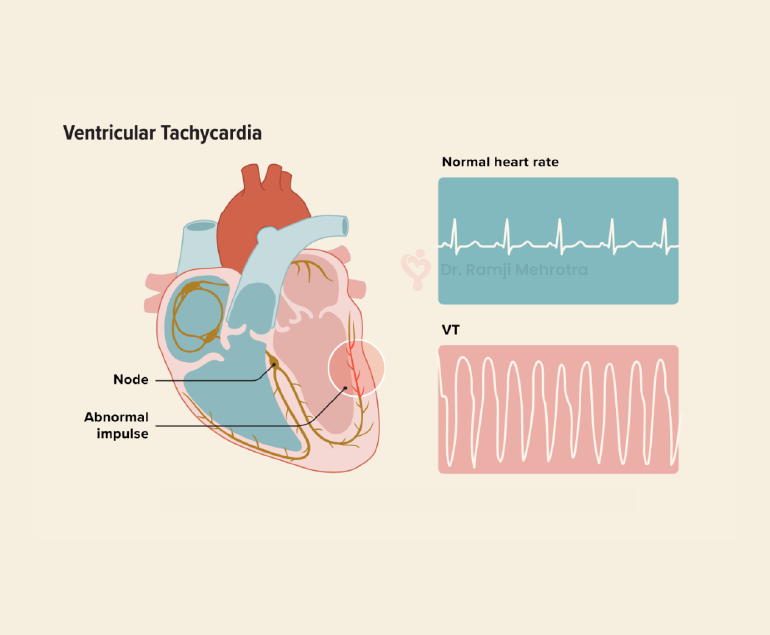
During pregnancy, the body undergoes significant changes to support fetal growth. Blood volume increases, heart rate rises, and the cardiovascular system works harder to meet the body’s increased oxygen and nutrient demands. For women with cardiovascular disease, these changes can aggravate their condition and lead to complications such as heart failure, arrhythmias, and thromboembolic events. Hypertension, in particular, can become more challenging to manage during pregnancy and is a significant risk factor for complications.
Risks for Fetus
The developing fetus relies on a well-functioning maternal cardiovascular system for oxygen and nutrient supply. Maternal cardiovascular disease can compromise blood flow to the placenta, potentially resulting in fetal growth restriction, preterm birth, or stillbirth. Additionally, certain medications used to manage cardiovascular conditions may have teratogenic effects on the developing fetus, highlighting the importance of careful medication management during pregnancy.
Management and Monitoring
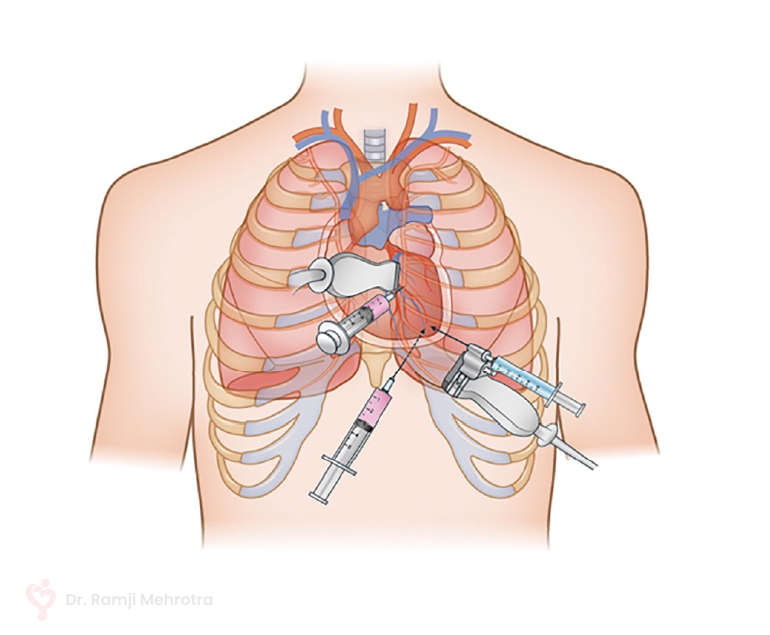
Managing cardiovascular disease during pregnancy requires a multidisciplinary approach involving obstetricians, cardiologists, and other specialists as needed. Individualized treatment plans are crucial, taking into account the specific cardiovascular condition, its severity, and the patient’s overall health. Medications may need to be adjusted or changed to minimize potential harm to the fetus while ensuring maternal well-being.
Frequent monitoring is essential throughout pregnancy. This includes regular check-ups to assess blood pressure, cardiac function, and fetal growth. Advanced imaging techniques like echocardiography and Doppler ultrasound can provide valuable insights into maternal and fetal well-being.
Delivery Planning
The mode of delivery should also be carefully planned. In many cases, vaginal delivery is safe and appropriate, but a caesarean section may be recommended if there are concerns about the mother’s cardiovascular stability or the fetus’s well-being. The timing of delivery may also be adjusted to optimize outcomes for both mother and baby.
Postpartum Care
The challenges of managing cardiovascular disease do not end with delivery. The postpartum period is a critical time, as the body undergoes significant physiological changes once again. Close monitoring should continue, and adjustments to medications and treatment plans may be necessary.
Conclusion
Pregnancy with pre-existing cardiovascular disease requires meticulous planning, close monitoring, and a collaborative healthcare team. While it can be associated with increased risks for both the mother and the fetus, with proper management and care, many women with cardiovascular disease can have successful pregnancies and healthy babies. Education, counseling, and ongoing support are vital for empowering women with cardiovascular disease to make informed decisions about family planning and to navigate the complex journey of pregnancy with confidence.