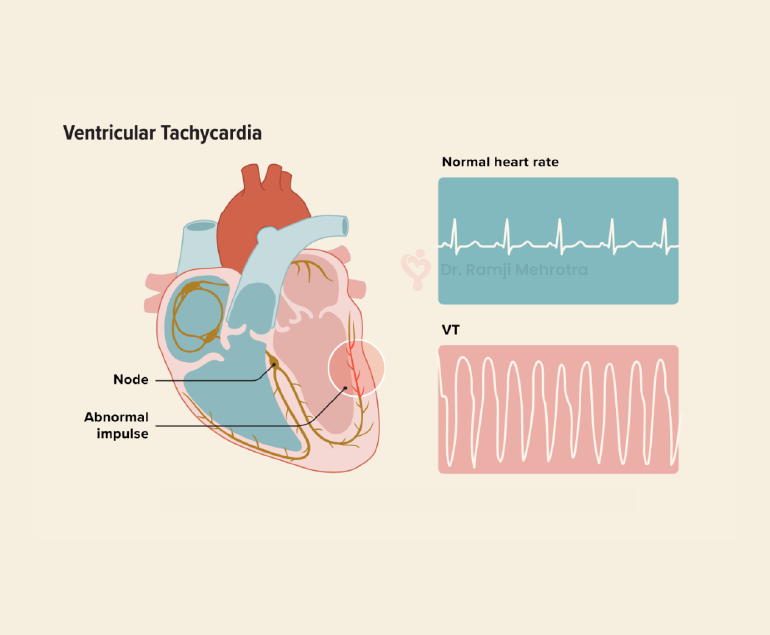
Ventricular tachycardia (VT) is a potentially life-threatening cardiac arrhythmia characterized by a rapid heartbeat originating in the ventricles, the lower chambers of the heart. In VT, the heart beats faster than the normal rate, usually over 100 beats per minute, and it can be sustained for longer periods, making it a serious medical condition that requires prompt attention and treatment.
Causes of Ventricular Tachycardia
VT typically results from abnormal electrical signals in the heart, often due to an underlying heart condition. Common causes include:
- Coronary Artery Disease (CAD): The most common cause of VT is CAD, which leads to insufficient blood flow to the heart muscle. This lack of oxygen can disrupt the heart’s electrical system, leading to arrhythmias like VT.
- Cardiomyopathy: Conditions like dilated or hypertrophic cardiomyopathy can cause changes in the heart’s structure and electrical system, increasing the risk of VT.
- Heart Attack: An acute myocardial infarction (heart attack) can scar heart tissue, creating areas where abnormal electrical impulses can arise.
- Valvular Heart Disease: Malfunctioning heart valves can affect blood flow, increasing the likelihood of arrhythmias, including VT.
- Electrolyte Imbalances: Abnormal levels of electrolytes (such as potassium, sodium, or calcium) can disrupt the heart’s electrical signals.
Symptoms
The symptoms of VT can vary in severity and may include:
- Palpitations: A strong, rapid heartbeat is a hallmark symptom of VT.
- Chest Pain: Some people may experience chest discomfort or pain during VT episodes.
- Dizziness or Lightheadedness: Insufficient blood flow to the brain can lead to these sensations.
- Shortness of Breath: Rapid heartbeats can reduce the heart’s efficiency, leading to breathlessness.
- Loss of Consciousness: In severe cases, VT can cause fainting or even sudden cardiac arrest.
Diagnosis
A proper diagnosis of VT involves a combination of medical history, physical examination, and diagnostic tests, including:
- Electrocardiogram (ECG or EKG): This test records the heart’s electrical activity and can identify VT patterns.
- Holter Monitor: A portable ECG device worn for an extended period can capture intermittent VT episodes.
- Electrophysiology Study (EPS): Invasive testing, where thin wires are inserted into the heart, can pinpoint the location and cause of VT.
- Echocardiogram: This ultrasound imaging of the heart can reveal structural abnormalities.
Treatment Options
The management of VT depends on its cause, severity, and the patient’s overall health. Treatment options may include:
- Medications: Antiarrhythmic drugs can help control VT episodes by stabilizing the heart’s electrical activity.
- Implantable Cardioverter-Defibrillator (ICD): For those at high risk of life-threatening VT, an ICD is surgically implanted to monitor and correct abnormal rhythms by delivering shocks when needed.
- Catheter Ablation: This procedure involves the use of catheters to target and destroy the abnormal heart tissue responsible for VT.
- Lifestyle Changes: Managing underlying conditions like CAD or cardiomyopathy through lifestyle modifications, such as diet, exercise, and smoking cessation, can reduce the risk of VT.
- Emergency Care: If VT leads to cardiac arrest, immediate defibrillation is crucial to restore normal rhythm and save a life.
Conclusion
Ventricular tachycardia is a serious cardiac arrhythmia that requires careful evaluation and management. Early diagnosis and appropriate treatment are essential to reduce the risk of life-threatening complications. Patients with a history of heart disease or risk factors should consult with the doctors regularly for them to monitor and address any cardiac issues, ultimately improving their overall heart health and quality of life.