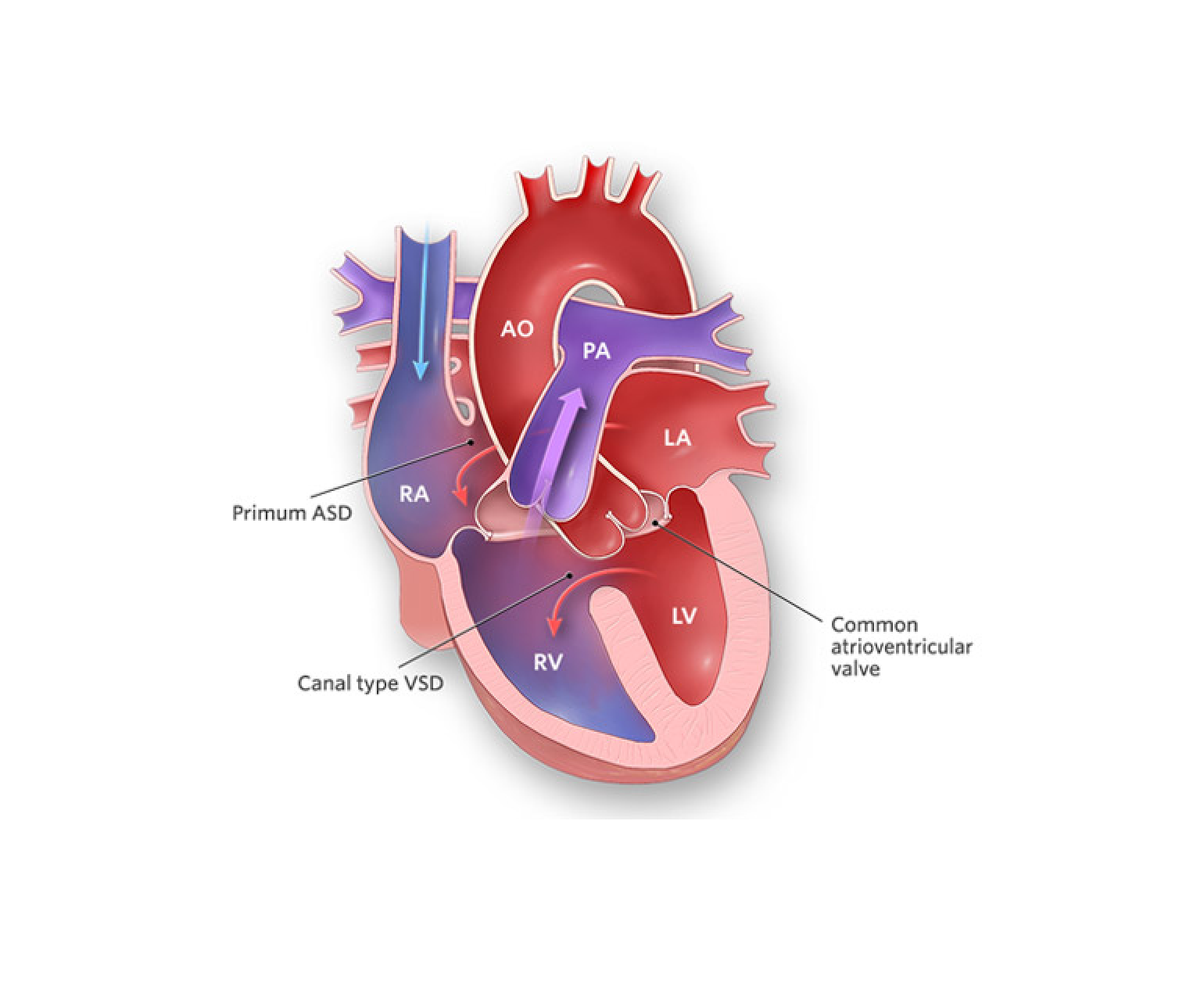
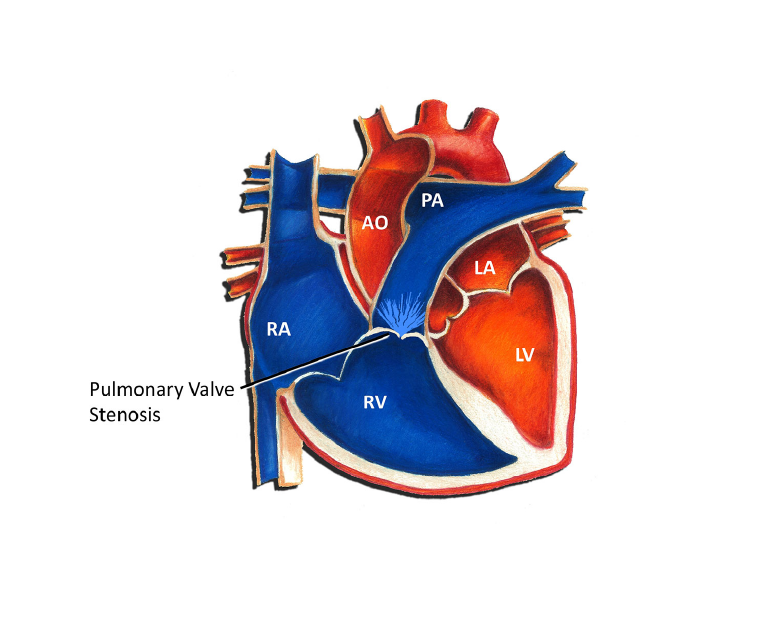
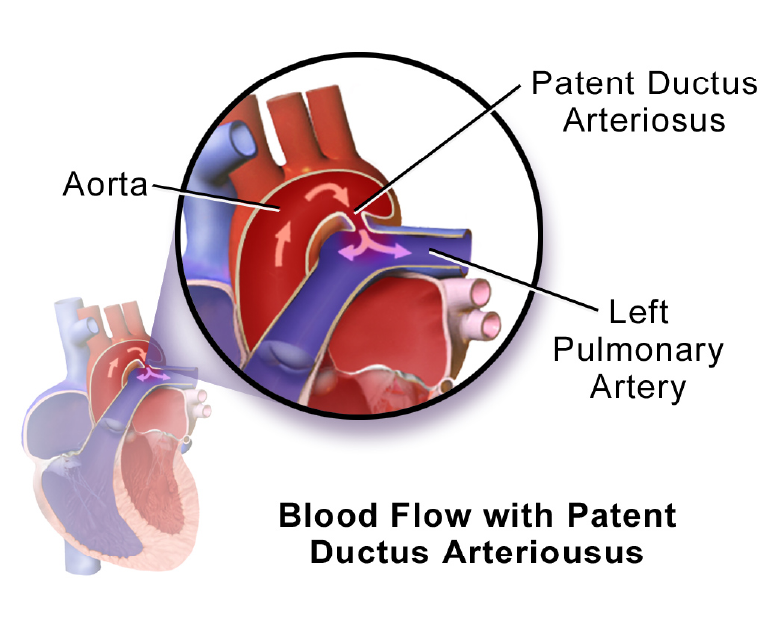
Complete atrioventricular canal defect (CAVC) is a rare congenital heart condition that occurs when there is a hole in the centre of the heart that affects the atria and ventricles. This condition is also known as an atrioventricular septal defect (AVSD), and it can cause a range of serious health problems if left untreated.
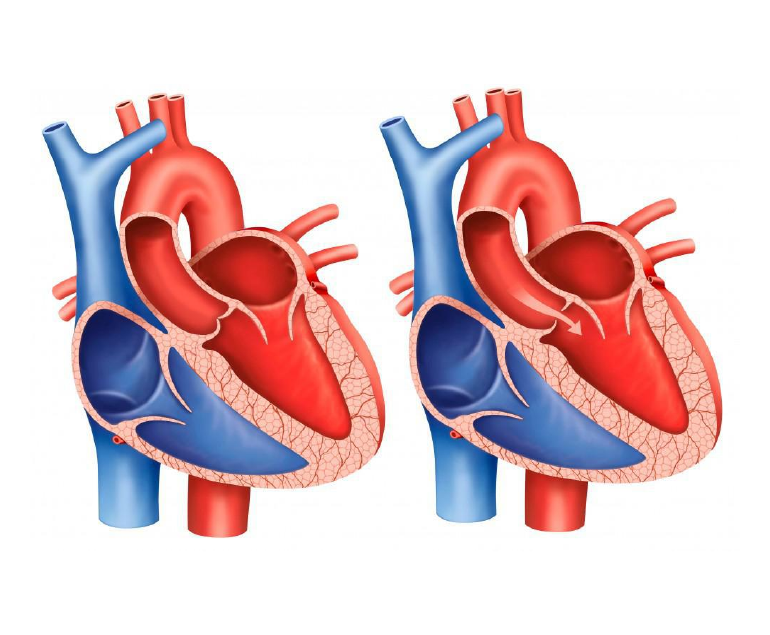
In a normal heart, there is a wall (septum) between the two atria and another wall between the two ventricles. These walls prevent the mixing of oxygen-rich and oxygen-poor blood. In CAVC, these walls are missing, and a large hole exists between the atria and ventricles. As a result, oxygen-rich blood mixes with oxygen-poor blood, leading to reduced oxygen levels in the body and heart failure over time.
Diagnosis of CAVC
CAVC is typically diagnosed in infancy or early childhood. Infants with CAVC may experience symptoms such as difficulty breathing, rapid breathing, and feeding difficulties. In some cases, babies with CAVC may also have low oxygen levels, which can cause a bluish tint to the skin (cyanosis).
The diagnosis of CAVC is usually confirmed through diagnostic tests such as an echocardiogram, which uses ultrasound waves to create images of the heart. Other tests that may be performed include an electrocardiogram (ECG) to evaluate the heart’s electrical activity and a chest X-ray to check for signs of heart enlargement.
Treatment
Treatment for CAVC usually involves surgery to close the hole in the heart and reconstruct the affected valves. This type of surgery is typically done in early infancy or early childhood, depending on the severity of the condition. In some cases, medication may be prescribed to manage symptoms such as heart failure or to prevent complications such as infection.
Long-term outlook
The long-term outlook for children with CAVC depends on the severity of the defect and the timing of treatment. In general, children who receive timely and appropriate treatment have a good prognosis and can live normal, healthy lives. However, in severe cases, CAVC can lead to heart failure, pulmonary hypertension, and other serious complications.
In addition to medical treatment, children with CAVC may require ongoing monitoring and care throughout their lives. This may include regular check-ups with a pediatric cardiologist, medication management, and follow-up diagnostic tests such as echocardiograms.
Conclusion
Complete atrioventricular canal defect is a rare but serious congenital heart condition that affects the atria and ventricles of the heart. Early diagnosis and appropriate treatment are crucial for managing the condition and preventing complications. If you suspect your child may have CAVC, it is important to seek medical attention promptly to ensure the best possible outcome.