Rheumatic heart disease (RHD) is a serious condition that affects the heart valves and is a result of complications from rheumatic fever. Although it is preventable and treatable, RHD continues to be a significant health burden in many developing countries, particularly among children and young adults.
Causes
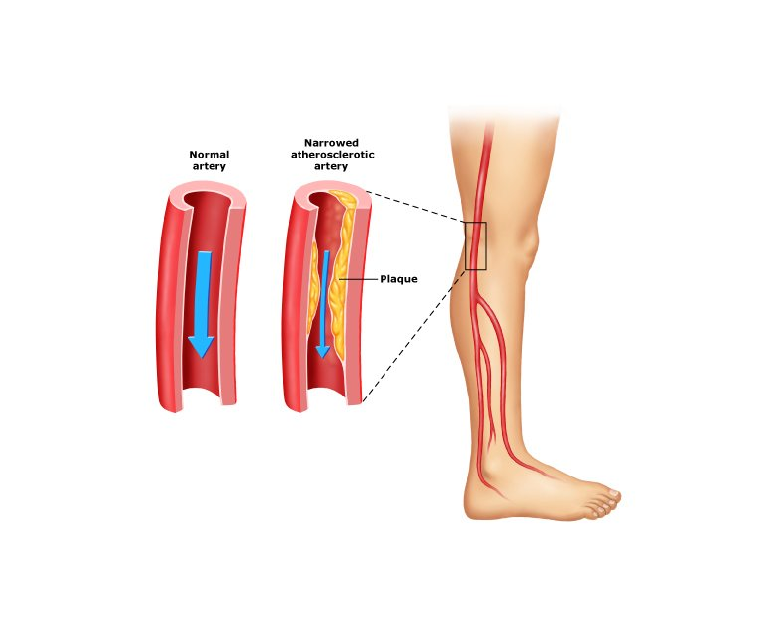
RHD is caused by an abnormal immune response to untreated or inadequately treated streptococcal throat infections, mainly caused by group A streptococcus bacteria. When these infections are not promptly treated with antibiotics, the body’s immune system can mistakenly attack its own tissues, including the heart valves. Over time, this can lead to scarring, thickening, and deformation of the valves, which impairs their ability to function properly.
Symptoms
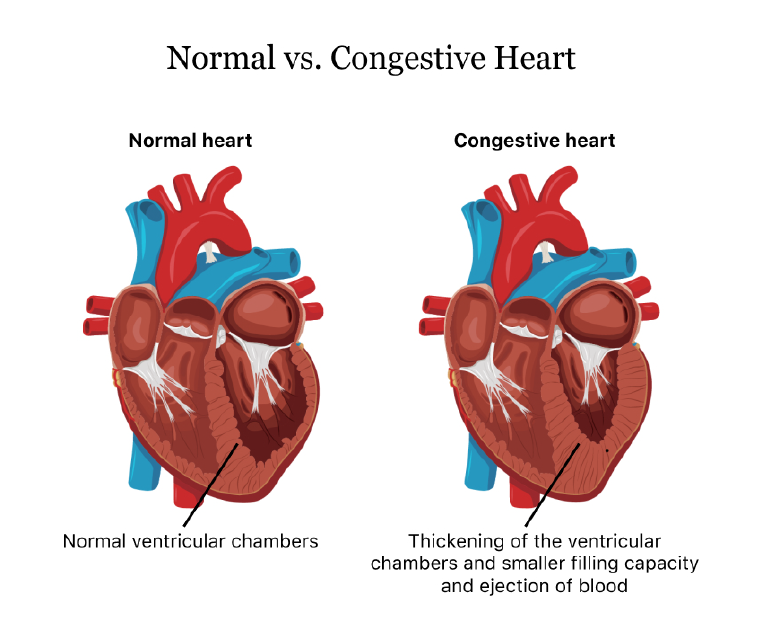
The symptoms of RHD can vary depending on the severity and location of valve damage. In the early stages, there may be no noticeable symptoms, but as the disease progresses, individuals may experience shortness of breath, chest pain, fatigue, palpitations, and swollen ankles or feet. In severe cases, heart failure and life-threatening complications, such as infective endocarditis or stroke, can occur.
Diagnosis & Treatment
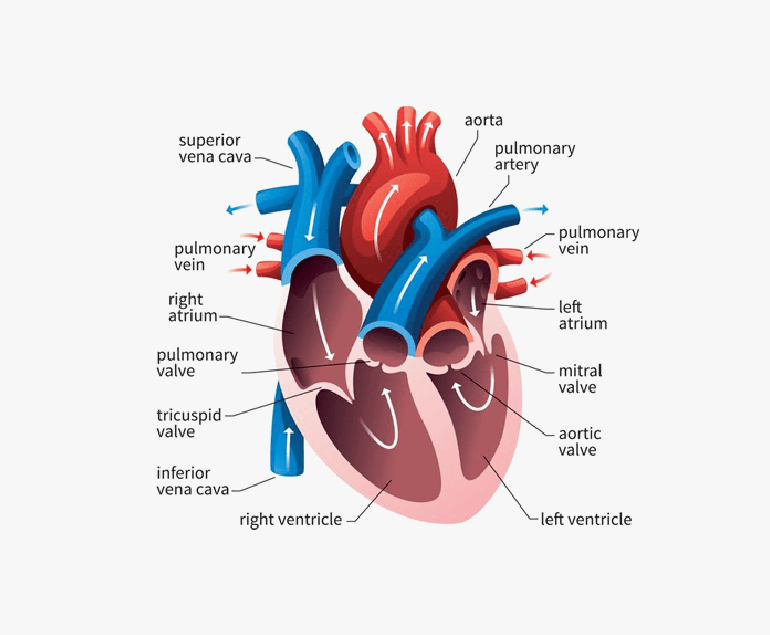
Diagnosing RHD typically involves a combination of medical history assessment, physical examination, echocardiography (ultrasound of the heart), electrocardiogram (ECG), and other imaging tests. These tests help evaluate the structure and function of the heart, identify valve abnormalities, and determine the extent of damage.
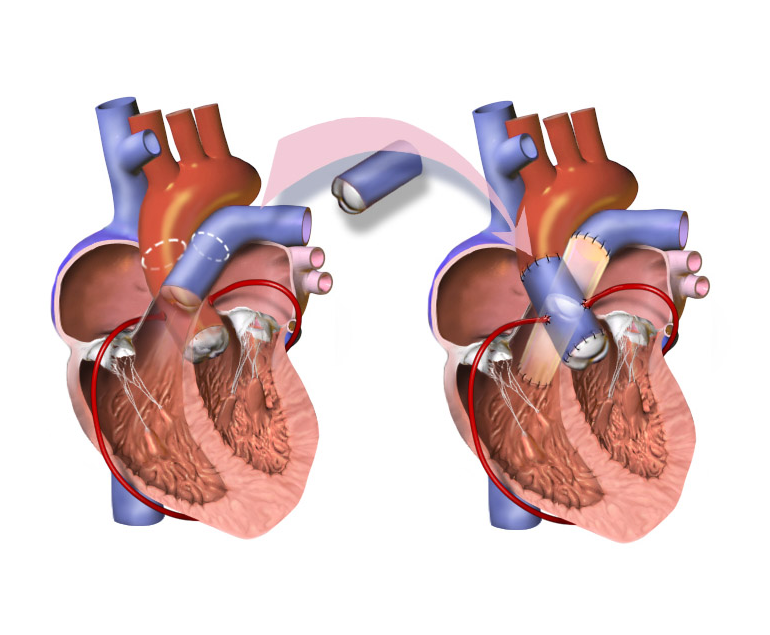
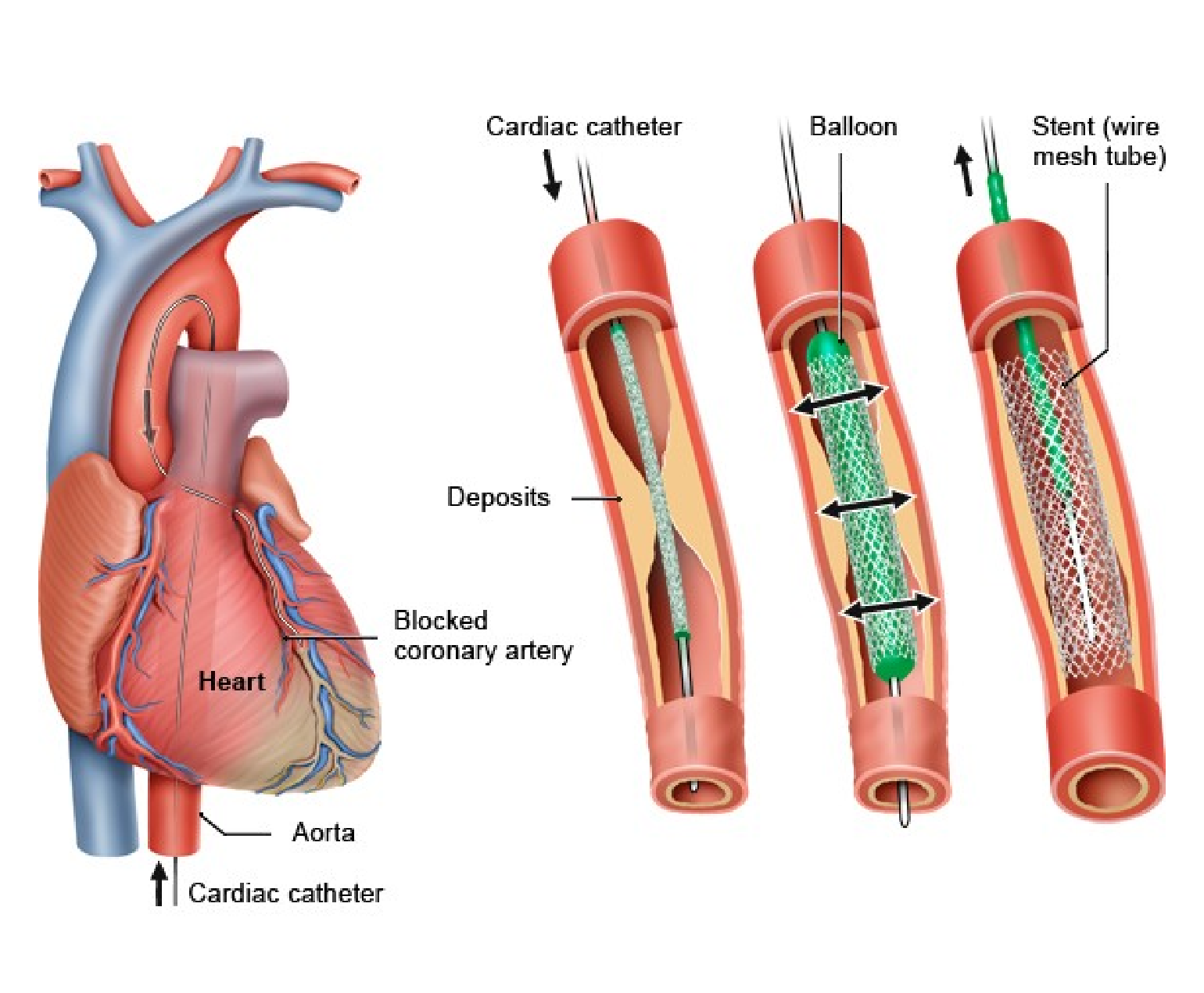
Treatment for RHD aims to manage symptoms, prevent disease progression, and reduce the risk of complications. Antibiotic prophylaxis is crucial to prevent recurrent streptococcal infections, which can trigger disease exacerbation. Medications, such as diuretics, beta-blockers, and anticoagulants, may be prescribed to manage symptoms and reduce the risk of blood clots.
Prevention
Preventing RHD begins with prompt and appropriate treatment of streptococcal throat infections. Administering antibiotics, such as penicillin, to individuals with streptococcal infections can prevent the development of rheumatic fever, thereby reducing the risk of RHD. Regular follow-up and secondary prophylaxis, which involves long-term antibiotic treatment, are essential for individuals who had rheumatic fever to prevent disease recurrence and progression.
Conclusion
Rheumatic heart disease is a preventable and treatable condition that continues to be a significant health concern in many parts of the world. Prompt and appropriate treatment of streptococcal throat infections, along with regular follow-up and secondary prophylaxis, are vital for preventing the development and progression of RHD. By prioritizing prevention, early detection, and comprehensive management, the impact of rheumatic heart disease can be minimised.