Cardiovascular conditions in older patients pose significant challenges due to the natural aging process and the increased prevalence of risk factors associated with advanced age. As individuals grow older, their cardiovascular system undergoes changes that can increase the likelihood of developing various heart-related disorders.
Some of the common cardiovascular conditions seen in older patients include:
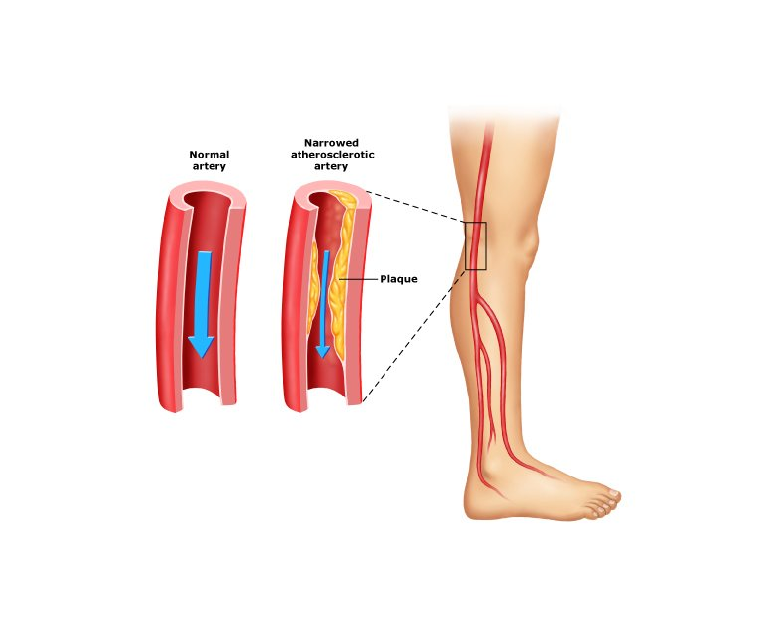
Coronary Artery Disease (CAD)
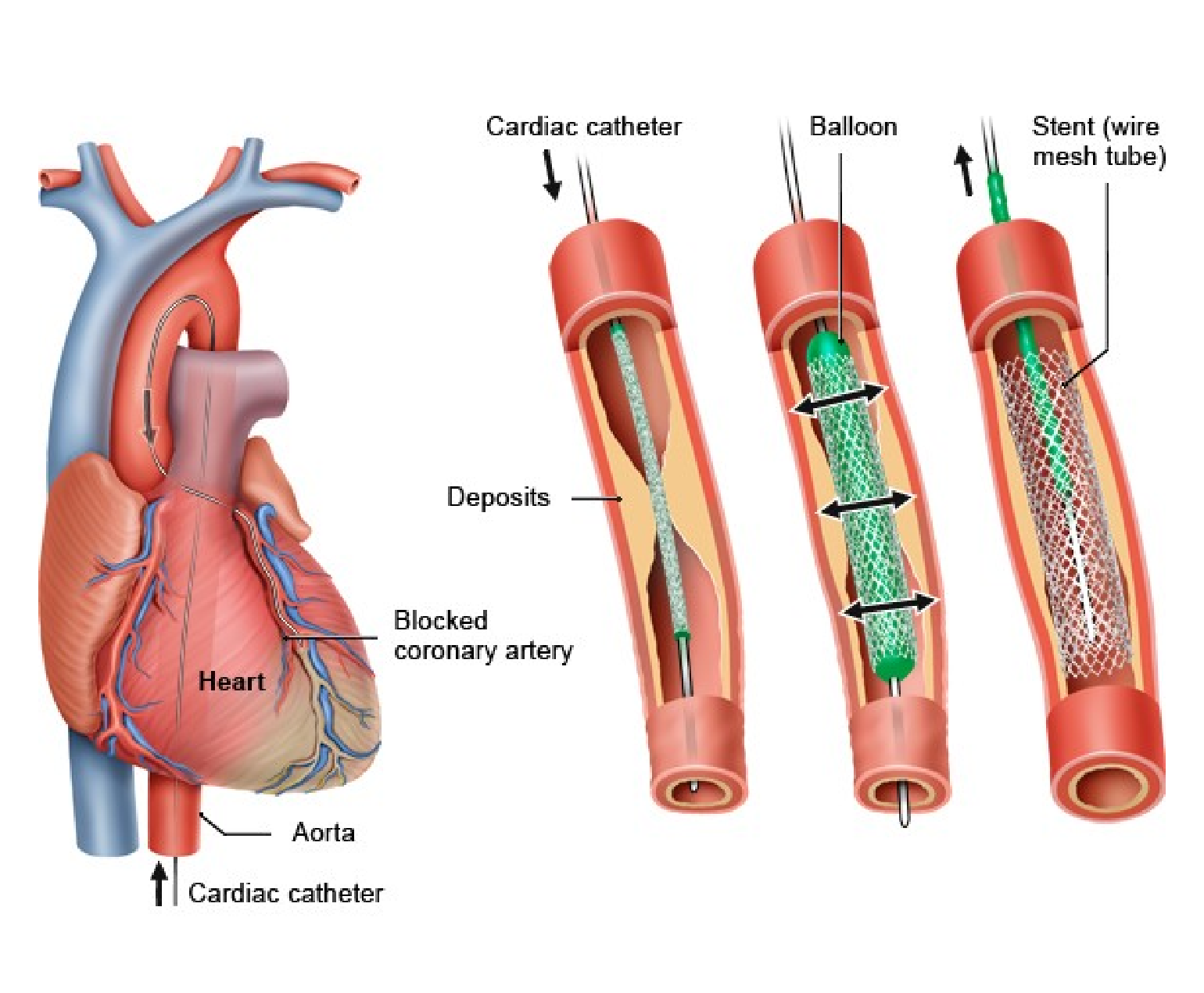
One of the most prevalent cardiovascular conditions in older adults is coronary artery disease (CAD). CAD occurs when the arteries that supply blood to the heart become narrowed or blocked due to atherosclerosis, the build-up of plaque. Older adults are more at risk to CAD due to factors such as prolonged exposure to risk factors like high blood pressure, high cholesterol, and smoking.
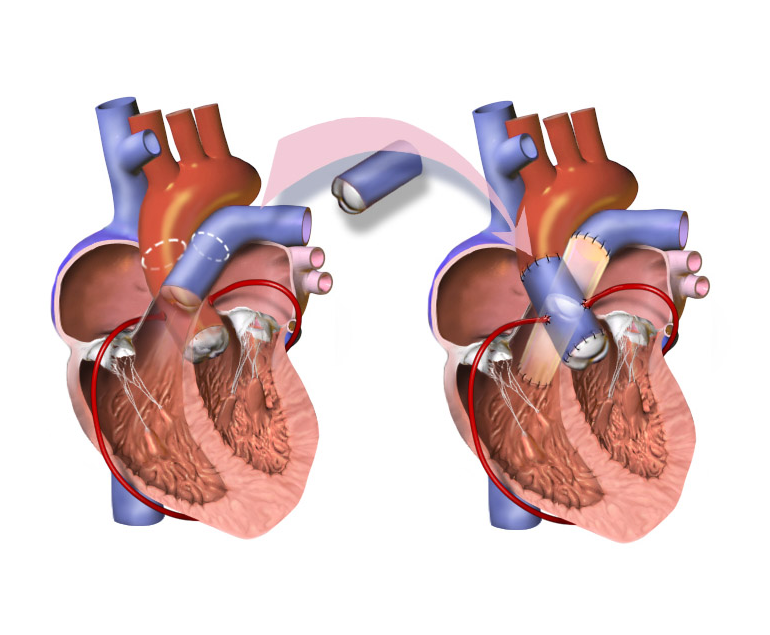
Diagnosis of CAD in older patients may be challenging because symptoms can be masked by other age-related conditions. Doctors employ diagnostic tools such as stress tests and cardiac imaging to confirm the diagnosis. Treatment typically involves a combination of lifestyle modifications, medication management, and, in severe cases, invasive interventions like angioplasty or bypass surgery.
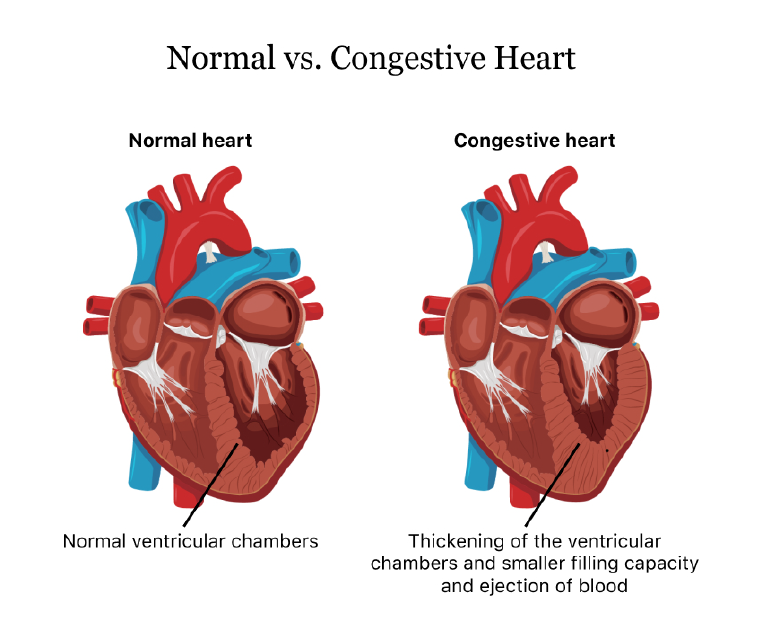
Heart failure
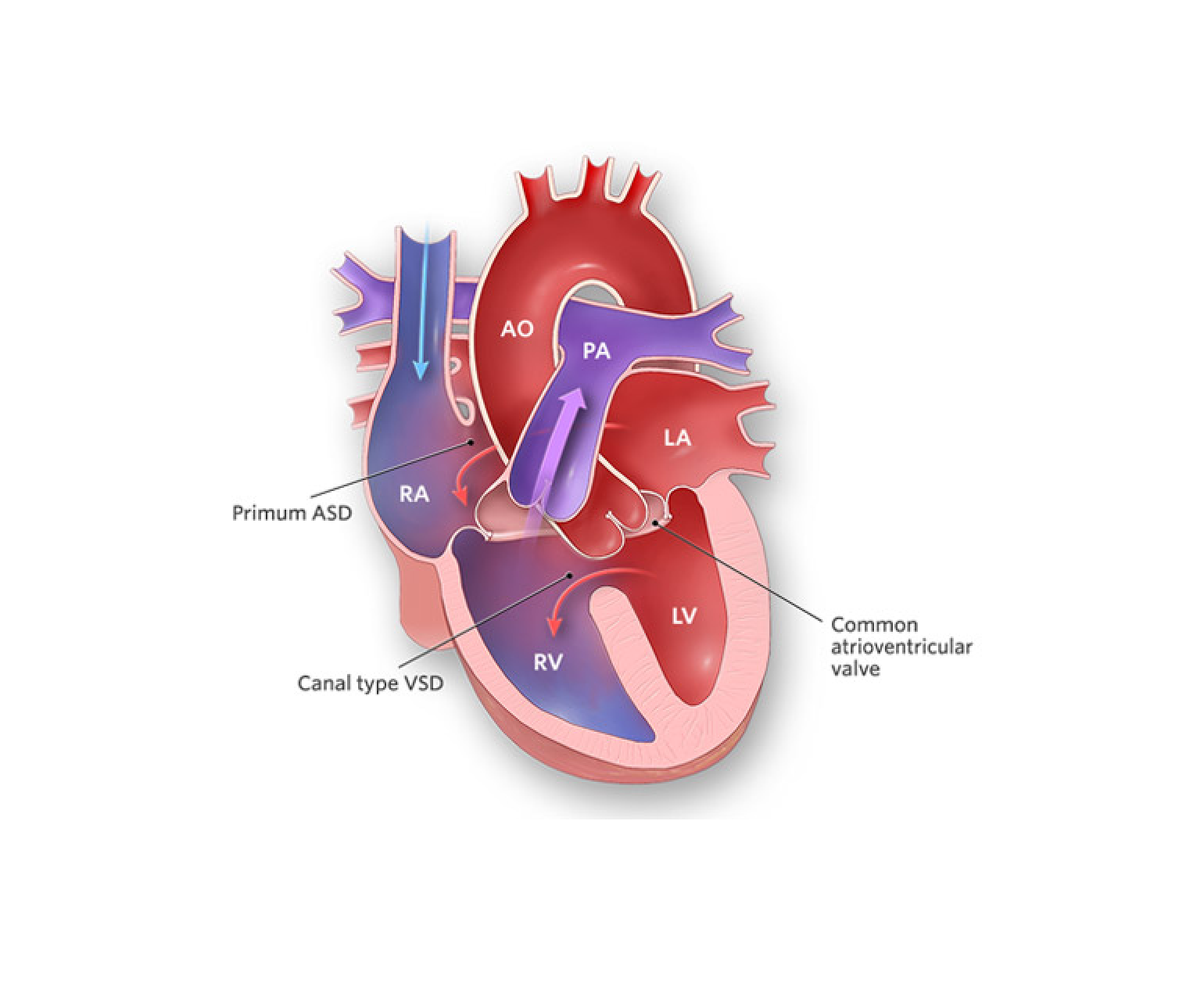
Heart failure is another common cardiovascular condition in older patients. It occurs when the heart is unable to pump blood efficiently, leading to symptoms such as shortness of breath, fatigue, and fluid retention. Age-related changes in the heart, such as reduced elasticity and stiffening of the cardiac muscles, increase the risk of heart failure.
Accurate diagnosis of heart failure requires a comprehensive assessment of symptoms, physical examination, and diagnostic tests like echocardiography. Treatment involves a combination of medications to manage symptoms and improve heart function, lifestyle modifications like fluid and salt restriction, and, in some cases, devices like pacemakers or implantable defibrillators.
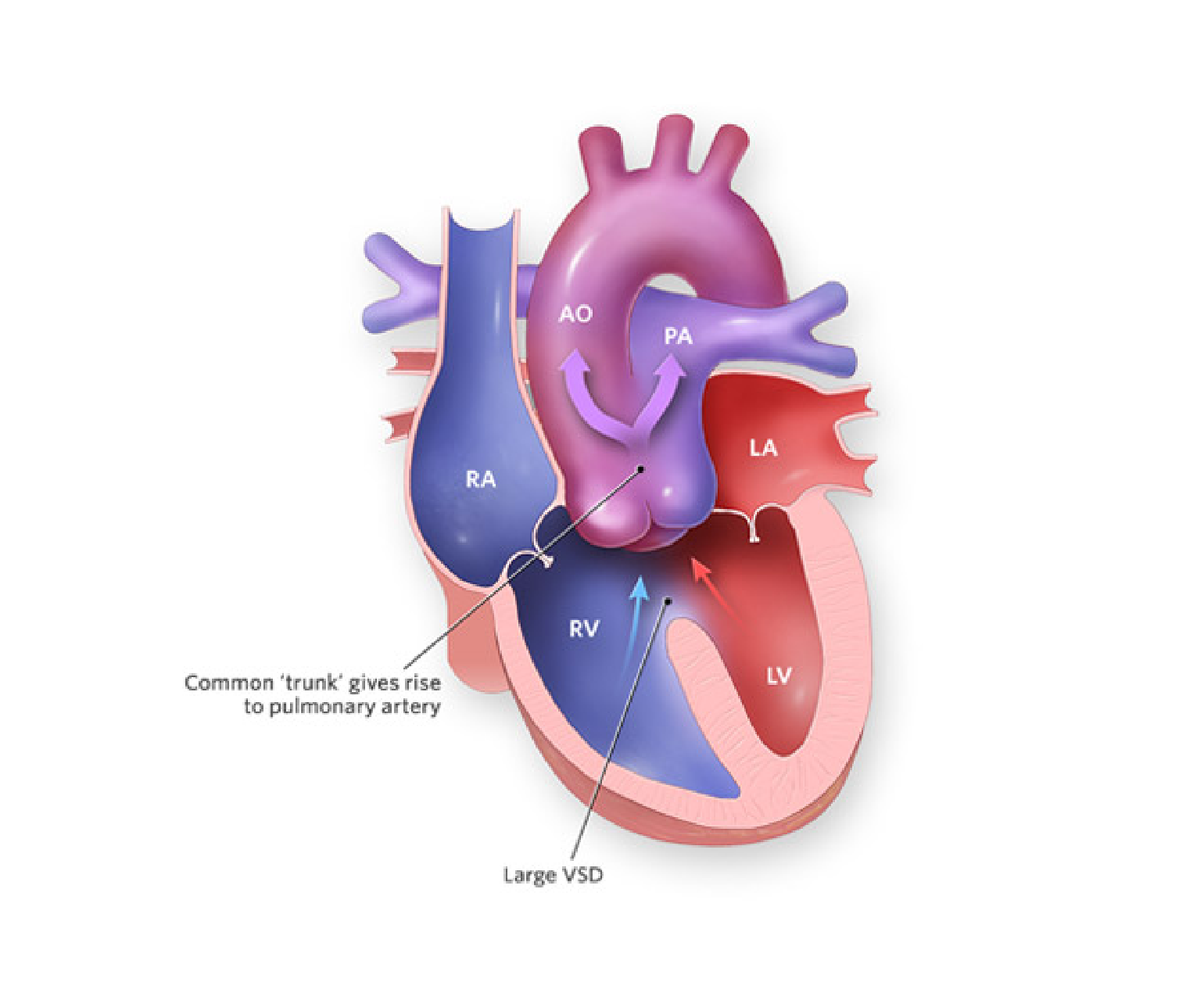
Arrhythmias
Arrhythmias, including atrial fibrillation (AF), are commonly encountered in older adults. AF, characterized by irregular and rapid heartbeat, is associated with an increased risk of stroke, heart failure, and other cardiovascular complications.
Advanced age is a significant risk factor for developing AF due to changes in the electrical conduction system of the heart. Diagnosis involves an electrocardiogram (ECG) and may require additional monitoring methods like Holter monitoring or event recorders. Management of AF in older patients aims to control heart rate, prevent blood clots with anticoagulant therapy, and restore normal heart rhythm when possible.
Hypertension
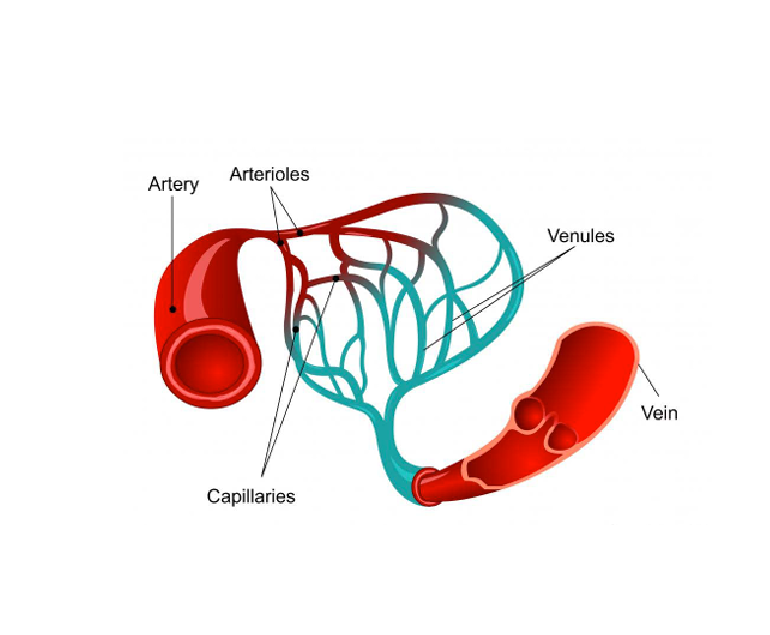
Hypertension, or high blood pressure, is highly prevalent in older adults and is a major risk factor for cardiovascular disease. Age-related changes in blood vessels, hormonal factors, and lifestyle habits contribute to the development of hypertension.
Effective management of hypertension in older patients involves lifestyle modifications, such as a heart-healthy diet and regular exercise, along with medications to achieve blood pressure targets. Close monitoring and regular follow-up are essential to ensure blood pressure control and prevent complications.
Conclusion
Cardiovascular conditions in older patients require a comprehensive and individualized approach to diagnosis and treatment. Age-related changes in the cardiovascular system increase the vulnerability of older adults to conditions like coronary artery disease, heart failure, arrhythmias, and hypertension. Addressing modifiable risk factors and promoting healthy lifestyle habits are essential for preventing and managing cardiovascular conditions in older patients.